Key Takeaways
- Vaginal surgery can address physical causes of sexual dysfunction like dyspareunia and vaginismus.
- Common procedures include vaginoplasty, perineoplasty, labiaplasty, and clitoral hood reduction.
- Success rates vary; realistic expectations and proper patient selection are crucial.
- Non‑surgical options such as pelvic floor therapy and hormonal treatment should be tried first or combined with surgery.
- Potential complications exist, so thorough pre‑op counseling and post‑op care are essential.
When pain or lack of pleasure turns intimacy into a chore, many wonder if a scalpel can fix the problem. vaginal surgery is a set of procedures that reshape or tighten the vaginal canal and surrounding tissues. It’s often suggested for women whose sexual dysfunction stems from anatomical issues that haven’t responded to conservative care.
Understanding Sexual Dysfunction
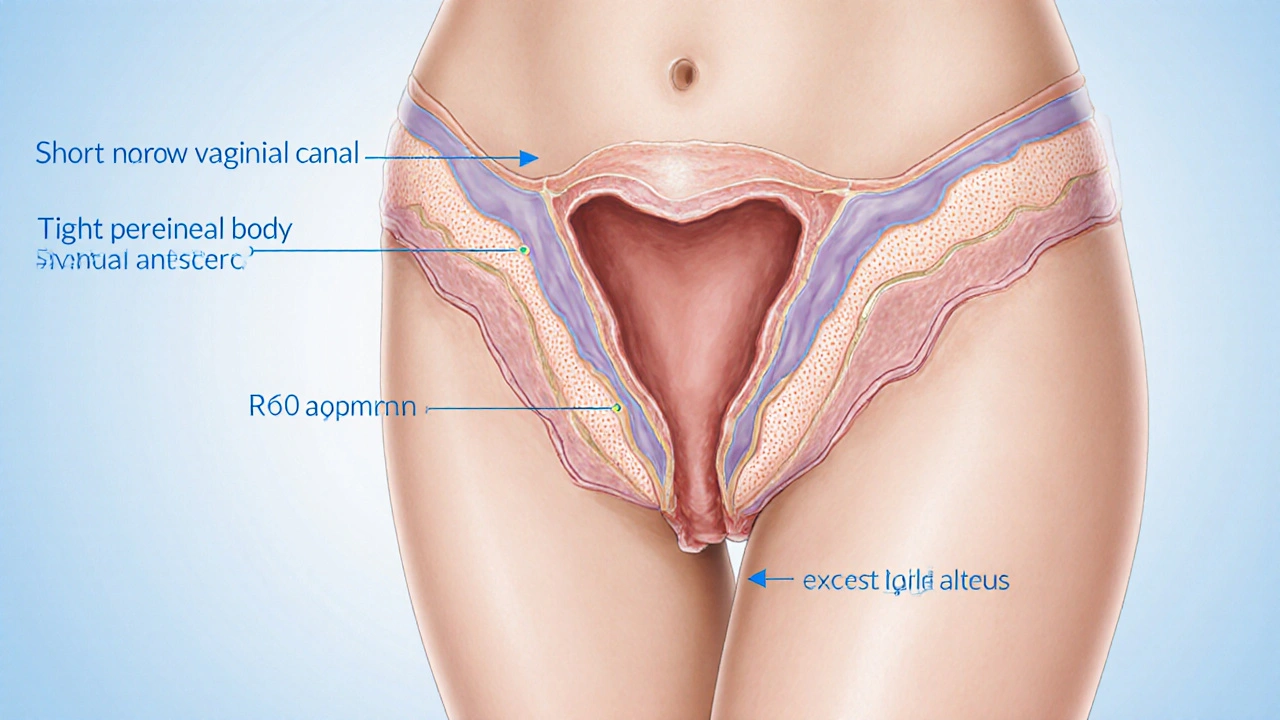
Sexual dysfunction is a broad term covering problems with desire, arousal, orgasm, or pain during intercourse. In women, the most common physical complaints are dyspareunia (painful intercourse) and vaginismus (involuntary muscle tightening). While psychological factors play a big role, structural abnormalities-like a short vaginal canal, excessive labial tissue, or scar tissue from previous childbirth-can be the root cause.
When Anatomy Affects Function
Think of the vagina as a tunnel that needs enough length and elasticity for comfortable penetration. Conditions that shorten the tunnel, such as post‑hysterotomy scarring or congenital vaginal agenesis, often lead to discomfort. Excessive labial tissue can cause friction, while a tight perineal body (the tissue between the vagina and anus) may trigger vaginismus. Identifying these issues usually involves a pelvic exam, sometimes complemented by imaging like pelvic MRI.
Types of Vaginal Surgery
Each surgical option targets a specific anatomical concern.
- Vaginoplasty lengthens and widens the vaginal canal, often using tissue grafts or flaps. It’s the go‑to for dyspareunia caused by a short vagina.
- Perineoplasty tightens the perineal body, reducing spasms that lead to vaginismus.
- Labiaplasty trims excess labial tissue, decreasing friction and improving aesthetics.
- Clitoral hood reduction can enhance clitoral stimulation for women experiencing reduced orgasmic pleasure.

How Surgery Helps
By restoring proper dimensions and relieving tightness, vaginal surgery removes the physical barrier to pleasurable intercourse. For example, a successful vaginoplasty can add 1‑2cm of depth, enough for most penetrative positions. Perineoplasty, on the other hand, relaxes the muscle reflex that causes involuntary tightening, allowing the woman to engage without pain.
Choosing Surgery - Decision Checklist
- Confirm that a physical cause has been identified by a qualified pelvic‑floor specialist.
- Attempt at least 3months of non‑surgical treatment (pelvic‑floor PT, lubricants, counseling).
- Discuss realistic outcomes with a board‑certified urogynecologist.
- Evaluate personal health factors-smoking, diabetes, obesity-which can affect healing.
- Ensure you have a supportive post‑op care plan (partner, time off work, follow‑up visits).
Recovery & What to Expect
Recovery timelines differ by procedure:
- Vaginoplasty: 4-6weeks for full healing; gentle dilation may be recommended.
- Perineoplasty: 2-3weeks; pelvic‑floor exercises start after the first week.
- Labiaplasty: 1-2weeks; scar care is essential.
During the first week, most surgeons advise abstaining from penetrative sex and using a water‑based lubricant for any activity. Pain should gradually subside, but a mild ache or tightness can linger for a month.

Non‑Surgical Alternatives & When to Combine
Before opting for scalpel work, many women benefit from:
- Pelvic floor physical therapy - a series of exercises and manual techniques that improve muscle tone and relax spasms.
- Topical estrogen creams for post‑menopausal thinning of vaginal tissue.
- Sex therapy or counseling to address anxiety and relationship factors.
- Lubricants and vaginal dilators for gradual desensitization.
Some patients combine PT with surgery-doing PT before and after the operation often boosts success rates to 80‑90%.
Risks & Complications
All surgeries carry risks. Common issues include infection, bleeding, and scarring. Specific to vaginal procedures are:
- Dyspareunia from over‑tightening (rare, but treatable with dilation).
- Change in sensation-some women report heightened or reduced feeling.
- Urinary or bowel dysfunction if nearby nerves are affected.
Choosing an experienced surgeon and following post‑op instructions cut these risks dramatically.
Comparing Surgical vs Non‑Surgical Treatments
| Aspect | Surgical Treatment | Non‑Surgical Treatment |
|---|---|---|
| Typical Success Rate (pain reduction) | 70‑90% | 30‑60% (depends on adherence) |
| Recovery Time | 2‑6weeks (procedure‑specific) | Immediate, but benefits accrue over weeks/months |
| Average Cost (US) | $5,000‑$12,000 | $150‑$500 per session (PT); $30‑$100 for lubricants |
| Invasiveness | High (incision, anesthesia) | Low (exercises, topical agents) |
| Long‑Term Maintenance | Periodic dilation, follow‑up exams | Ongoing PT, home exercises |
Frequently Asked Questions
Can vaginal surgery restore sexual desire?
Surgery mainly addresses physical barriers. Desire is mostly driven by hormonal and psychological factors, so most doctors recommend counseling or hormonal therapy alongside any procedure.
How long does a vaginoplasty take?
The operation itself usually lasts 1-2hours, depending on complexity and whether tissue grafts are used.
Is anesthesia risky for these procedures?
Most surgeons use regional (spinal) or general anesthesia. Risks are low for healthy adults, similar to other outpatient surgeries. Pre‑op screening minimizes complications.
Will I need dilation after surgery?
Many patients use vaginal dilators for 10‑15minutes daily during the first month to maintain depth and prevent scar contracture.
Can I try pelvic floor therapy first?
Absolutely. Most guidelines recommend at least three months of targeted PT before considering surgery, unless a severe anatomical defect is already identified.
What are the most common complications?
Infection, bleeding, over‑tightening, and temporary changes in sensation are the top three. Early detection and prompt treatment keep outcomes favorable.
How do I find a qualified surgeon?
Look for board‑certified urogynecologists or pelvic reconstructive surgeons with specific experience in vaginoplasty and perineoplasty. Patient reviews and before‑after photos can help gauge expertise.

BJ Anderson
October 12, 2025 AT 00:06While the idea of fixing intimacy with a scalpel sounds tempting, it’s crucial to remember that the body isn’t a mechanical puzzle you can simply re‑assemble. Surgery can indeed relieve structural issues, but the drama often begins in the weeks of recovery and the possibility of new complications. If the underlying emotional or relational factors aren’t addressed, the “fix” may feel hollow. In short, think of surgery as a tool, not a miracle.
Alexander Rodriguez
October 17, 2025 AT 05:06Surgery works for clear anatomical problems, but it isn’t a first‑line solution for most women.
Abhinav Sharma
October 22, 2025 AT 12:53First off, the pelvic floor is a highly adaptable muscular canvas, not a static tunnel. Targeted physical therapy can re‑educate those muscles, often restoring depth and comfort without a knife. When you combine a few weeks of PT with gentle dilators, many patients report a 70‑80% drop in pain levels 😊. Surgery should be reserved for cases where scar tissue or congenital narrowing is proven, and even then, a multidisciplinary approach yields the best outcomes. Think of the body as an orchestra; every instrument must be in tune before the soloist shines. 🎵
Welcher Saltsman
October 27, 2025 AT 22:26Honestly, give the non‑surgical route a solid try – it’s low risk, and you might be surprised at how much it helps.
april wang
November 2, 2025 AT 11:46Vaginal surgery occupies a contentious space in sexual health, balancing genuine anatomical correction against the risk of over‑medicalization. First, it is essential to recognize that dyspareunia and vaginismus often stem from a complex interplay of tissue integrity, neuromuscular control, and psychological context. When a clinician identifies a tangible structural deficit-such as a short vaginal canal after a radical hysterectomy-surgical lengthening can restore the mechanical environment necessary for comfortable penetration. However, the success of any procedure hinges on a pre‑operative evaluation that includes pelvic floor assessment, hormonal status, and an honest discussion of expectations. Patients should be educated that the goal is not necessarily to achieve “perfect” sexual performance, but to eliminate pain and improve quality of life. Post‑operative care is just as critical; dilation protocols, pelvic floor exercises, and ongoing counseling can prevent scar contracture and reinforce new muscle patterns. Moreover, the financial burden of surgery, often ranging from five to twelve thousand dollars, can be prohibitive for many, especially when insurance coverage varies widely. In contrast, a regimen of physical therapy, lubricants, and cognitive‑behavioral therapy may be incrementally less costly and carries a negligible risk profile. A common misconception is that surgery guarantees a return to the libido; desire is largely driven by hormonal and emotional factors, which remain untouched by scalpel work. Therefore, integrating sex therapy with any surgical plan can address the missing pieces. From a clinical perspective, a multidisciplinary team-including a urogynecologist, pelvic physio specialist, and mental health professional-optimizes outcomes and reduces complication rates. Finally, the ethical dimension cannot be ignored: clinicians must avoid suggesting surgery as a cosmetic fix for societal pressures on female sexuality. In sum, while surgical options have a legitimate place, they should be pursued after exhausting conservative measures, with realistic expectations and a solid support network in place.
Vishnu Raghunath
November 8, 2025 AT 03:53Oh sure, just cut a little, and all your relationship woes magically disappear.
Aparna Dheep
November 13, 2025 AT 22:46While brevity has its charm, reducing a multifaceted issue to a single sentence overlooks the nuanced biopsychosocial model that underpins sexual health. One must consider hormone levels, previous trauma, and even cultural narratives before labeling surgery as merely “the second line.”
Nicole Powell
November 19, 2025 AT 20:26Presenting these procedures as routine fixes reeks of profit‑driven medicine; many women are steered toward expensive operations without being fully informed of the modest success rates.
Ananthu Selvan
November 25, 2025 AT 20:53Enough with the fluff – if you’re not willing to put in the work, surgery is just a waste of cash.
Nicole Chabot
December 2, 2025 AT 00:06Hey there, taking the time to research all options is the smartest move you can make. Knowledge is power!
Sandra Maurais
December 8, 2025 AT 06:06Statistical analyses reveal that adverse event rates for vaginoplasty hover around 4‑5%, a figure that many promotional materials conveniently downplay. Moreover, the long‑term satisfaction curves flatten after the first year, suggesting that initial enthusiasm may be transient 📉. Prospective patients should demand raw data rather than cherry‑picked success stories.
Michelle Adamick
December 14, 2025 AT 14:53From a pelvic reconstructive standpoint, leveraging autologous tissue flaps during vaginoplasty optimizes mucosal integration and mitigates contracture risk 🚀. Coupled with bio‑feedback‑guided perineal training, these protocols synergistically elevate functional outcomes and patient‑reported quality‑of‑life indices.
Edward Glasscote
December 21, 2025 AT 02:26Physical therapy can actually stretch the tissue enough to avoid surgery.
Gaurav Joshi
December 27, 2025 AT 16:46Contrary to the melodrama, the majority of complications are minor and easily managed, making the risk‑benefit ratio more favorable than popular media suggests.
Jennifer Castaneda
January 3, 2026 AT 09:53There’s a hidden agenda in the medical community to pathologize normal variance in female anatomy, turning everyday discomfort into a marketable disease. By branding any deviation as “dysfunction,” pharmaceutical and surgical industries lock patients into lifelong dependency on costly interventions. The data on long‑term outcomes is murky, and many studies are funded by the very companies that profit from the procedures. It’s prudent to remain skeptical and demand independent research before committing to an operation that could alter one’s bodily autonomy.
Annie Eun
January 10, 2026 AT 05:46Isn’t it fascinating how the quest for a “perfect” intimate experience can lead us down a rabbit hole of endless procedures? Yet, true fulfillment often lies beyond the operating room, within the realms of self‑acceptance and open communication.
Jay Kay
January 17, 2026 AT 04:26Surgery works if anatomy is the issue
Franco WR
January 24, 2026 AT 05:53Reading through the comprehensive overview, I’m struck by the balanced emphasis on both surgical precision and holistic care. Your point about multidisciplinary teams resonates strongly; integrating physio, mental health, and surgical expertise creates a safety net that many patients lack. The acknowledgment of cost barriers is also vital-financial stress can exacerbate anxiety, undermining recovery. Moreover, your reminder that desire is multifactorial underscores the need for realistic expectations, which can prevent post‑op disappointment. I appreciate how you highlighted ethical considerations, steering clinicians away from cosmetic exploitation. Overall, this nuanced perspective equips readers with a roadmap that honors both body and mind.