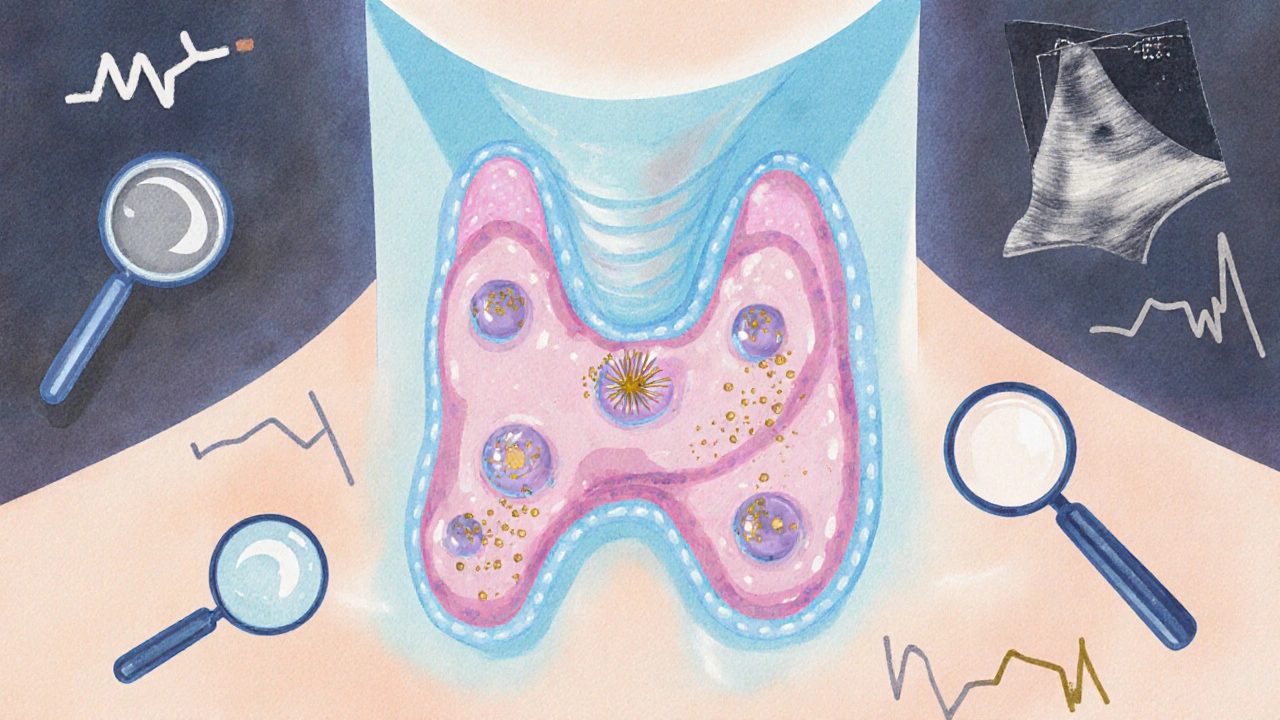
More than half of adults over 60 have a thyroid nodule-most never know it. These small lumps in the thyroid gland are so common that finding one during an ultrasound is almost routine. But when you hear the word thyroid nodule, panic can creep in. Is it cancer? Do I need surgery? The truth is, 90 to 95% of thyroid nodules are harmless. The real challenge isn’t finding them-it’s knowing which ones actually need action.
What Makes a Thyroid Nodule Suspicious?
Not all nodules are created equal. The key to avoiding unnecessary procedures lies in spotting the warning signs. Ultrasound is the first and most important tool. A good ultrasound can tell you more about a nodule than a physical exam ever could. Malignant nodules often show specific features: tiny calcium deposits (microcalcifications), irregular or spiky edges, and a darker appearance on the scan (hypoechogenicity). These aren’t guesses-they’re patterns backed by decades of research. For example, microcalcifications show up in about 56% of papillary thyroid cancers, the most common type. Irregular margins appear in 83% of malignant cases. When you see these together, the risk jumps. Benign nodules, on the other hand, tend to look smoother, often with fluid inside (cystic), or have a spongy, honeycomb-like texture. Pure cysts-fluid-filled sacs-are almost always harmless. Even nodules with some solid parts can be benign if they lack those red-flag features.Size Matters, But Not the Way You Think
You’ve probably heard that nodules over 1 cm need a biopsy. That’s true-but it’s not the whole story. The American Thyroid Association says you should consider a biopsy if a nodule is 1 cm or larger and has suspicious ultrasound features. If it’s 1.5 cm or bigger and looks normal, biopsy is still recommended. And if it’s 2 cm or larger, even if it looks fine, you should get it checked. But size alone doesn’t tell you everything. A 1.2 cm nodule with clear cancer signs is more concerning than a 2.5 cm nodule that looks like a benign colloid nodule. That’s why doctors don’t just measure-they analyze.Growth Rate: The Silent Red Flag
One of the most powerful predictors of cancer isn’t what a nodule looks like at first-it’s how it changes over time. A 2017 study in the Journal of Clinical Endocrinology & Metabolism found that if a nodule grows more than 2 mm per year in at least two directions, the chance of it being cancerous goes up sharply. For every extra 2 mm per year beyond that, the risk climbs even higher. Benign nodules grow slowly-often less than 1 mm per year. In a five-year study, only 14.2% of benign nodules even doubled in size. Malignant ones? They’re faster. And that’s why follow-up ultrasounds matter. If your nodule was 1.1 cm last year and now it’s 1.5 cm, that’s a 4 mm increase in one dimension. If it also grew in another direction, you’re past the 2 mm/year threshold. That’s a trigger.What Happens During a Thyroid Biopsy?
Fine-needle aspiration (FNA) is the standard test. It’s quick-usually under 15 minutes-and done right in the doctor’s office. An ultrasound guides a thin needle into the nodule. A small sample of cells is pulled out and sent to a lab. The results are sorted using the Bethesda System, a six-category classification that tells you the cancer risk:- Category 1: Nondiagnostic (1-4% risk) - Not enough cells. Repeat biopsy needed.
- Category 2: Benign (0-3% risk) - Almost certainly harmless. Monitor with ultrasound.
- Category 3: Atypia of undetermined significance (5-15% risk) - Unclear. Often needs molecular testing.
- Category 4: Follicular neoplasm (15-30% risk) - Could be cancer. Surgery often recommended.
- Category 5: Suspicious for malignancy (60-75% risk) - Highly likely cancer. Surgery usually follows.
- Category 6: Malignant (97-99% risk) - Cancer confirmed. Treatment plan starts now.

What If the Biopsy Is Unclear?
About 20-30% of biopsies land in Category 3 or 4-indeterminate. That’s where things get messy. Many patients end up with unnecessary surgery because doctors don’t know what to do next. That’s why molecular testing exists. Tests like Afirma GSC or ThyroSeq v3 analyze the DNA and RNA in the nodule cells. They can tell you whether the nodule is likely benign or malignant, even when the cells look ambiguous. A 2020 study showed these tests cut unnecessary surgeries by 35% in indeterminate cases. ThyroSeq v3, approved by the FDA in 2022, checks 112 genes. It has 94% sensitivity and 93% specificity-meaning it rarely misses cancer and rarely says cancer when it’s not there. If your biopsy is indeterminate, ask if molecular testing is an option. It’s covered by most insurance.Benign vs. Cancerous: What’s Actually in There?
Most benign nodules are either follicular adenomas (noncancerous tumors), colloid nodules (clumps of stored thyroid hormone), or cysts. These don’t spread. They don’t kill. They might cause discomfort if they get big-swallowing trouble, hoarseness, a feeling of something stuck in your throat-but they’re not cancer. Cancerous nodules? Almost all are papillary thyroid cancer (80%). It grows slowly, often spreads to neck lymph nodes, but it’s highly treatable. Follicular cancer (10-15%) rarely spreads to lymph nodes but can travel to lungs or bones. Rarer types like medullary or anaplastic cancer are aggressive but make up less than 5% of cases. The scary part? Most thyroid cancers don’t cause symptoms until they’re advanced. You won’t feel sick. You won’t lose weight. You might not even notice the nodule until your doctor sees it on an ultrasound.When Is Biopsy Avoidable?
Not every nodule needs a needle. If you’re over 60 and have a small (under 1 cm), purely cystic nodule with no suspicious features, your doctor might just watch it. The same goes for nodules found incidentally during a CT or MRI scan for something else. And here’s the twist: we’re diagnosing way more thyroid cancer than we used to. Since 1975, incidence has jumped 15-fold. But death rates haven’t changed. Why? Because we’re finding tiny, slow-growing cancers that would never have caused harm. This is called overdiagnosis. Dr. Gilbert Welch from Dartmouth calls it “finding ghosts.” Many of these tiny cancers (under 1 cm) stay stable for years. A 2021 JAMA Surgery study showed that 87% of small papillary cancers didn’t grow over five years of monitoring. That’s why active surveillance is now a recommended option for low-risk cases-especially in older patients.
What Comes After the Biopsy?
If your nodule is benign and not causing symptoms, you’ll likely get an ultrasound every 6 to 12 months for the first couple of years. If it doesn’t grow, you can space out the checks. If it’s cancerous, you’ll be referred to a thyroid surgeon. Most people get a lobectomy-removal of half the thyroid. Some need a total thyroidectomy. After surgery, you’ll take thyroid hormone replacement for life. But most people return to normal life with no major changes. If you’re in the indeterminate zone and molecular testing says benign, you can avoid surgery entirely. Studies show the risk of cancer is less than 3% after a negative molecular test.What About New Technologies?
Ultrasound elastography measures how stiff a nodule is-cancerous tissue tends to be harder. It’s 92% sensitive and 88% specific, but not widely used yet. AI tools like ThyroidAI, cleared by the FDA in 2022, can analyze ultrasound images and flag suspicious features. They’re not replacing doctors-they’re helping them. One study showed AI matched expert radiologists in accuracy 89% of the time. Radiofrequency ablation (RFA) is now being tested for large benign nodules that cause pressure symptoms. Early results from the THYROID-TRUST trial show RFA reduces nodule volume by 78% in a year-with far fewer complications than surgery.Who Should Be Worried?
Women are three times more likely than men to develop thyroid nodules. Risk increases with age. If you’ve had radiation to your head or neck (even as a child), your risk is higher. Family history of thyroid cancer also matters. But here’s the thing: if you have no symptoms, no family history, no radiation exposure, and your nodule is small and looks benign on ultrasound-you’re probably fine. You don’t need to rush into surgery. You don’t need to panic. What you need is a clear plan: ultrasound, follow-up, and smart testing-not fear.Are all thyroid nodules cancerous?
No. About 90 to 95% of thyroid nodules are benign. Most people never even know they have one. Only 5-10% turn out to be cancerous, and even then, most are slow-growing and highly treatable.
When should a thyroid nodule be biopsied?
Biopsy is typically recommended if the nodule is 1 cm or larger with suspicious ultrasound features, 1.5 cm or larger without suspicious features, or 2 cm or larger regardless of appearance. Growth of more than 2 mm per year in two directions is also a strong reason to biopsy, even if the nodule is smaller.
Can a benign thyroid nodule become cancerous?
It’s extremely rare. Benign nodules like follicular adenomas or colloid nodules don’t turn into cancer. However, a new cancer can develop separately in the thyroid. That’s why ongoing monitoring with ultrasound is important-even if a nodule is labeled benign.
What does an indeterminate biopsy result mean?
An indeterminate result (Bethesda Category 3 or 4) means the cells look unusual but aren’t clearly cancerous. About 20-30% of biopsies fall into this range. Molecular testing (like ThyroSeq or Afirma) can often clarify whether the nodule is likely benign or malignant, helping avoid unnecessary surgery.
Is thyroid cancer deadly?
Most thyroid cancers, especially papillary and follicular types, are not deadly. The 10-year survival rate is over 98% when caught early. Even if it spreads to lymph nodes, it’s usually treatable. Only rare types like anaplastic thyroid cancer are aggressive and hard to treat.
Can I avoid surgery if my nodule is cancerous?
For very small, low-risk papillary cancers (under 1 cm), active surveillance-regular ultrasounds without immediate surgery-is now an accepted option. Studies show most of these tumors don’t grow over five years. Surgery is still the standard for larger or more aggressive cancers.

Kihya Beitz
November 14, 2025 AT 10:48So let me get this straight - we’re doing biopsies on 95% of people who have something that’s basically a harmless pimple in their neck? I got a nodule at 58, didn’t even know it was there until my MRI for a migraine. Now I’m being pushed into a needle job like I’m a lab rat. Meanwhile, my cousin got a 3cm nodule and they just watched it for 7 years. It’s still there. She’s alive. We’re all just being scared into procedures now.
Jennifer Walton
November 15, 2025 AT 08:17Overdiagnosis is the silent epidemic. We treat ghosts like they’re threats.
John Foster
November 16, 2025 AT 16:21It’s not just about nodules. It’s about the entire medical-industrial complex turning every biological anomaly into a revenue stream. The thyroid is just the latest frontier in fear-based medicine. We’ve turned the human body into a checklist of potential disasters. And the worst part? The people who benefit from this system never have to live with the consequences. They don’t lie awake wondering if their biopsy was a mistake. They just file the claim, collect the fee, and move on to the next patient.
Edward Ward
November 17, 2025 AT 06:25I appreciate how thorough this breakdown is - especially the part about molecular testing. I had an indeterminate biopsy last year, and my doctor didn’t even mention ThyroSeq until I asked. It’s wild how much depends on whether your doctor is up to date or just following the old playbook. The fact that a test with 94% sensitivity and 93% specificity exists and still isn’t automatic is a failure of the system. Insurance coverage helps, but only if you know to ask. And most patients don’t. We need better patient education, not just better tech.
Andrew Eppich
November 19, 2025 AT 03:10It is irresponsible to suggest that active surveillance is appropriate for all small nodules. Cancer is cancer. Once it is present, it must be removed. The idea of waiting and watching is dangerous. If your child had a tumor, would you wait to see if it grows? No. You act. Medicine should be decisive, not hesitant.
Jessica Chambers
November 19, 2025 AT 19:04My nodule was 1.8cm. Looked fine. No growth. Doctor said "watch it." I did. Two years later, still nothing. Meanwhile, my cousin got a biopsy for a 0.7cm nodule with microcalcifications. Turned out benign. We’re all just playing Russian roulette with healthcare now. 🤷♀️
Shyamal Spadoni
November 20, 2025 AT 03:02you know what they dont tell you? the thyroid is controlled by the government through the water supply. all these "nodules" are just the side effect of fluoride and 5g. the real cancer is the system that wants you to trust them. they dont want you to know that natural iodine and seaweed can shrink them. they want you to pay for biopsies and hormones. its all a scam. i read this on a forum in 2017 and now im 100% sure. the truth is hidden. they even use ultrasound to confuse you. its just a magnet trick. dont believe the lies.
Ogonna Igbo
November 21, 2025 AT 23:44In Nigeria we don't have ultrasound machines in most clinics. We just feel the neck. If it's big and hard, we say it's cancer. If it's soft, we say it's just a bump. No one dies from thyroid cancer here because no one gets diagnosed. You live or you die. No biopsies. No labs. No insurance. Maybe that's better. At least we don't get scared by machines that lie.
BABA SABKA
November 23, 2025 AT 04:00Let’s be real - if your nodule is under 1cm and looks like a colloid nodule, you’re fine. The real issue is that radiologists are overinterpreting everything. They see a speck of calcium and go full CSI. I’ve seen cases where a 0.8cm nodule got a biopsy because the tech said it looked "slightly irregular." That’s not medicine. That’s fear-driven billing. RFA for benign nodules? Brilliant. Why cut out half your gland when you can zap it? The system just needs to catch up.
Chris Bryan
November 25, 2025 AT 03:14This is all part of the globalist agenda. The WHO, FDA, and Big Pharma want you dependent on hormones and biopsies. They’ve been pushing thyroid cancer overdiagnosis since the 90s to sell Synthroid. You think your nodule is benign? It’s a trap. They want you on lifelong medication. Don’t fall for it. Go natural. Stop eating soy. Stop drinking fluoridated water. Take selenium. You don’t need a needle.
Jonathan Dobey
November 26, 2025 AT 15:00The thyroid is the body’s thermostat. When it’s tampered with - by stress, by toxins, by corporate medicine - it whispers warnings. But we don’t listen. We drill into it with needles. We dissect it with scalpels. We replace it with synthetic hormones. We’ve forgotten that the body doesn’t make mistakes. If a nodule forms, it’s a signal. Not a disease. Not a tumor. A message. And we’re too busy scanning, biopsying, and billing to hear what it’s trying to say. The real cancer isn’t in the gland. It’s in our relationship with healing.
ASHISH TURAN
November 28, 2025 AT 08:02My mom had a nodule at 65. No symptoms. Ultrasound showed cystic with smooth edges. Doctor said watch and wait. Five years later, still the same size. She’s fine. No surgery. No meds. Just regular checkups. I think this article nails it - most people don’t need to panic. Just get the right info and stay calm.
Ryan Airey
November 30, 2025 AT 02:37Stop calling it "overdiagnosis." That’s just a fancy word for cowardice. If you find cancer, you remove it. Period. Waiting for it to grow is playing Russian roulette with your life. The fact that you’re even considering surveillance for cancer shows how broken medicine has become. You wouldn’t do that with a skin lesion. Why treat the thyroid differently? It’s the same tissue. Same rules. No exceptions.
Hollis Hollywood
December 1, 2025 AT 18:34I just want to say how much I appreciate this post. I’ve been terrified since my ultrasound last year. I’m 52, no family history, no radiation, just a 1.2cm nodule with a tiny bit of microcalcification. I was ready to schedule surgery until I read about molecular testing. My doctor didn’t bring it up - I had to Google it. I got the ThyroSeq test. It came back benign. I cried. Not because I was scared of cancer - but because I realized how alone I felt in this process. No one warned me that the system doesn’t always guide you. You have to fight for your own care. Thank you for giving me the language to ask the right questions.
Aidan McCord-Amasis
December 2, 2025 AT 19:4395% benign? Cool. So why am I paying $3k for a needle? 🤡