Pelvic Floor Therapy: What It Is, How It Helps, and What You Can Expect
When your pelvic floor muscles, a group of muscles that support the bladder, bowel, and reproductive organs. Also known as pelvic floor muscles, they weaken—whether from pregnancy, aging, surgery, or chronic strain—it can lead to leaks, pain, or discomfort. Pelvic floor therapy, a targeted form of physical therapy designed to strengthen, relax, or retrain these muscles is often the first non-drug solution doctors recommend. It’s not just for women after childbirth. Men recovering from prostate surgery, older adults with bladder control issues, and even athletes with chronic pelvic pain all benefit from it.
This therapy isn’t about doing a hundred Kegels a day. It’s about understanding how your muscles work, when to squeeze, and when to let go. A trained therapist uses hands-on techniques, biofeedback, and sometimes electrical stimulation to map out what’s going wrong. If your muscles are too tight, they’ll teach you how to release them. If they’re too weak, they’ll build strength slowly and safely. It’s common to see results in 6 to 12 weeks, and many people avoid surgery entirely by sticking with it. Urinary incontinence, the unintentional loss of urine is one of the most frequent reasons people seek this therapy. But it also helps with pelvic pain, a broad term covering discomfort in the lower abdomen, genitals, or rectum—whether from endometriosis, interstitial cystitis, or muscle tension.
What you’ll find in the posts below aren’t just generic advice. They’re real comparisons and practical insights on how pelvic floor therapy connects to other health issues. You’ll see how it ties into recovery from cancer treatments, how muscle spasms can worsen bladder control, and why stress plays a bigger role than most people realize. There’s no fluff here—just clear, direct information from people who’ve been through it, and experts who’ve seen what works. Whether you’re just starting to wonder if this could help you, or you’ve been told to try it and don’t know where to begin, this collection gives you the facts you need to move forward.
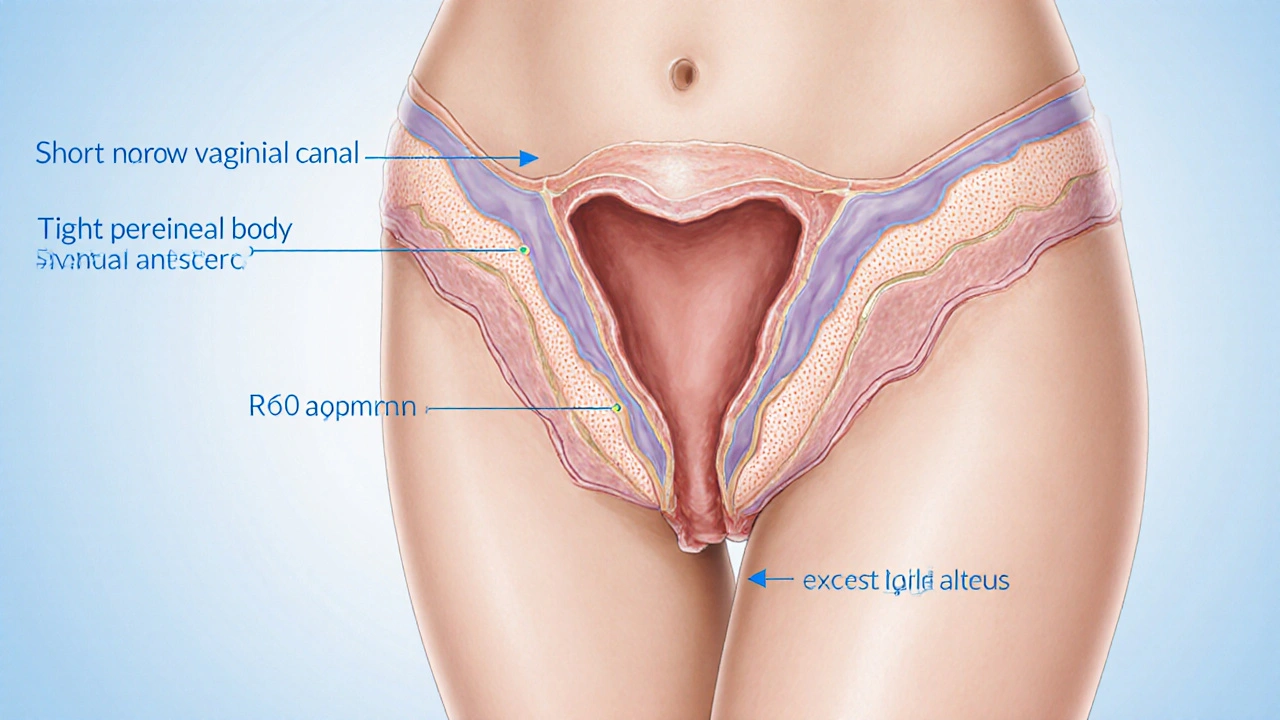
Vaginal Surgery’s Role in Treating Sexual Dysfunction - Benefits, Risks, and Alternatives
Explore how vaginal surgery can relieve dyspareunia and vaginismus, compare surgical and non‑surgical options, and learn the risks, recovery, and decision checklist.
READ MORE