When you're pregnant and struggling with depression or anxiety, the question isn't just whether to take an SSRI - it's whether not taking one might be riskier. For many women, this isn't a theoretical debate. It's a daily decision that affects their survival, their baby's health, and their ability to bond with their newborn. The truth? The risks of untreated depression during pregnancy often outweigh the known risks of SSRIs - but only if you understand the real numbers, not the headlines.
What Are SSRIs, and Why Are They Used in Pregnancy?
SSRIs - selective serotonin reuptake inhibitors - are the most commonly prescribed antidepressants today. Drugs like sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac) work by increasing serotonin levels in the brain. Serotonin helps regulate mood, sleep, and appetite. For someone with moderate to severe depression, this isn't a luxury - it's a lifeline. About 1 in 7 pregnant women experience depression or anxiety serious enough to need treatment. Left untreated, these conditions don't just make pregnancy harder - they can be deadly. According to CDC data from 2022, suicide accounts for 20% of all pregnancy-related deaths in the U.S. That’s more than hemorrhage or high blood pressure. And it’s not just about the mother. Untreated depression increases the risk of preterm birth by more than double, lowers birth weight, and makes postpartum depression far more likely.The Real Risks: Numbers That Matter
When people talk about SSRI risks, they often cite scary percentages. But percentages without context are misleading. Let’s break it down with actual numbers. Persistent Pulmonary Hypertension of the Newborn (PPHN) - a rare but serious lung condition - affects 1 to 2 out of every 1,000 babies in the general population. With SSRI use in the third trimester, that number rises to 3 to 6 per 1,000. That’s a relative increase of about 80%, but the absolute risk is still less than 1%. Compare that to untreated depression, which increases preterm birth risk by 120% - a much larger threat. Preterm birth happens in about 9.5% of pregnant women with depression who aren’t on medication. For those taking SSRIs, it’s 12.5%. At first glance, that sounds bad. But when researchers adjust for how severe the depression was to begin with - the real driver of risk - the difference shrinks to almost nothing. In fact, women with severe depression who stop their meds have a higher chance of preterm birth than those who stay on them. Birth defects are another big concern. Paroxetine (Paxil) is the only SSRI with a clear link to heart defects, increasing the risk from 0.5% to about 0.7-1%. That’s a small absolute increase. For all other SSRIs - including sertraline, the most commonly used - large studies of over 1.8 million births found no meaningful rise in major birth defects.The Bigger Picture: What Happens When You Stop
The biggest mistake many women make is stopping their SSRI cold turkey because they’re afraid of the baby. That’s dangerous. A 2022 JAMA Psychiatry study showed that women who stop SSRIs during pregnancy have a 4.3 times higher chance of their depression coming back. In fact, 92% of those who quit relapsed. Only 21% of those who kept taking their medication had a recurrence. Relapse doesn’t just mean feeling sad. It means inability to eat, sleep, care for yourself, or bond with your baby. It means higher risk of substance use - 25% of untreated depressed pregnant women use alcohol or drugs, compared to 8% of those on treatment. And then there’s postpartum depression. If you had depression during pregnancy and didn’t treat it, your chance of postpartum depression jumps to 14.5%. If you were treated with an SSRI? That drops to 4.8%. That’s a 67% reduction in risk.
Which SSRI Is Safest?
Not all SSRIs are the same. Sertraline is the first-line choice for pregnancy because it has the lowest placental transfer rate - meaning less of the drug crosses to the baby. Studies show cord blood levels are nearly equal to the mother’s, which is actually better than drugs that build up in the fetus. It’s also the SSRI with the lowest risk of PPHN. Citalopram and escitalopram are also considered safe. Fluoxetine stays in the body longer, so it’s often used when adherence is a concern, but it can accumulate in the baby, leading to more neonatal adaptation symptoms. Paroxetine? Avoid it. The cardiac defect risk, though small, is real and consistent across studies. Even if you’re not in your first trimester, switching to sertraline is recommended if you’re still on paroxetine.What About Long-Term Effects on the Child?
This is where things get murky. Some studies suggest children exposed to SSRIs in utero may have slightly higher rates of anxiety or depression by age 15. One Columbia University study found 28% of these children developed depression by adolescence, compared to 12% in children whose mothers had depression but didn’t take SSRIs. But here’s the catch: those same children’s mothers had more severe depression. And genetics play a huge role. A 2021 Lancet study that controlled for family history - including whether the father had depression - found no link between SSRIs and autism or major developmental delays. The risk, if any, appears tied more to the mother’s mental illness than the medication. The NIH’s 2023 review concluded: “The available data do not support a causal link between SSRI exposure and long-term neurodevelopmental harm.” That doesn’t mean we ignore the possibility - it means we weigh it against the known harm of untreated illness.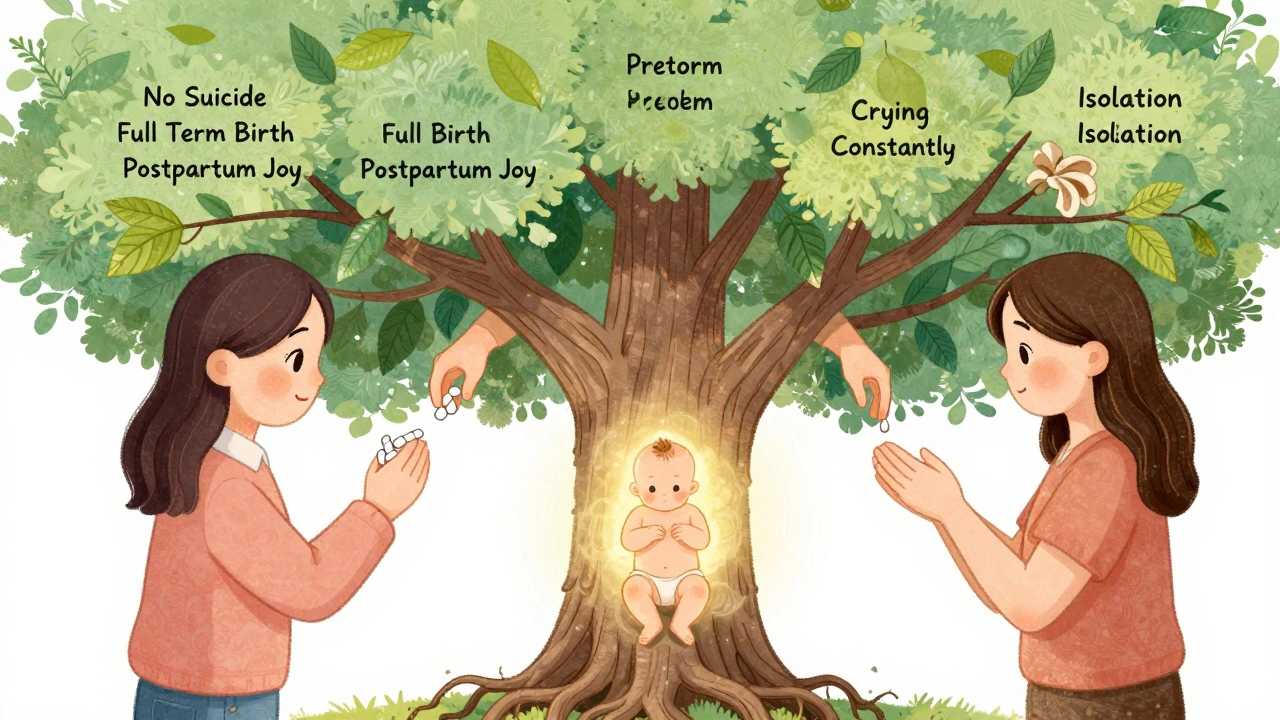
What Should You Do If You’re Pregnant and on an SSRI?
If you’re already taking an SSRI and find out you’re pregnant, do not stop. Talk to your doctor immediately. Here’s what to expect:- Stick with your current medication if it’s working - switching can trigger relapse.
- If you’re on paroxetine, switch to sertraline as soon as possible.
- Use the lowest effective dose. Many women do fine on 50mg of sertraline daily.
- Monitor for gestational hypertension - it’s slightly more common with SSRIs (8.5% vs. 6.2% in non-users), so weekly blood pressure checks after 20 weeks are recommended.
- Don’t stop abruptly. Withdrawal symptoms - dizziness, nausea, “brain zaps” - happen in 73% of women who quit cold turkey.
What If You’re Not on Medication But Think You Need It?
If you’re pregnant, feeling hopeless, unable to sleep, or crying most days - you don’t have to suffer alone. Depression isn’t weakness. It’s a medical condition. Talk to your OB-GYN or a perinatal psychiatrist. Therapy (like CBT) can help, but for moderate to severe cases, medication is often necessary. SSRIs are not a cure-all, but they’re one of the most effective tools we have. The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) both say: for women with moderate to severe depression, the benefits of SSRIs outweigh the risks. That’s not an opinion - it’s based on data from millions of pregnancies.The Bottom Line
You’re not choosing between a safe drug and a dangerous one. You’re choosing between two risks: the risk of a medication with low, measurable side effects - and the risk of untreated depression, which carries far higher odds of harming you and your baby. Sertraline is safe. Fluoxetine is safe. Paroxetine is not. Stopping your meds is riskier than staying on them. The data doesn’t lie. The fear does. Your mental health matters as much as your baby’s physical health. Treating depression isn’t selfish - it’s the most protective thing you can do for your child.Are SSRIs safe during pregnancy?
Yes, for most women. Sertraline, citalopram, escitalopram, and fluoxetine are considered safe and are not linked to a significant increase in major birth defects. Paroxetine should be avoided due to a small increased risk of heart defects. The absolute risks of SSRIs are low, and the risks of untreated depression - including suicide, preterm birth, and postpartum depression - are far greater.
Can SSRIs cause autism or developmental delays in my child?
Current evidence doesn’t support a clear link. Some early studies suggested a small increase in autism risk, but those didn’t account for family history or severity of maternal depression. A large 2021 Lancet study that controlled for genetics found no significant association. The American College of Obstetricians and Gynecologists and the NIH both conclude that any potential neurodevelopmental risk is outweighed by the benefits of treating maternal depression.
What’s the safest SSRI to take while pregnant?
Sertraline (Zoloft) is the first-line choice. It has the lowest placental transfer rate, the lowest risk of PPHN, and the most data supporting its safety. It’s also effective for both depression and anxiety, which are common in pregnancy. Citalopram and escitalopram are also good options. Fluoxetine is safe but stays in the body longer, which can lead to more newborn symptoms.
Should I stop my SSRI if I’m pregnant?
No - unless your doctor advises it. Stopping SSRIs abruptly increases your risk of depression relapse by over 4 times. About 92% of women who quit relapse. Untreated depression raises the risk of preterm birth, low birth weight, and postpartum depression. If you’re concerned, talk to your provider about switching to a safer SSRI like sertraline or adjusting your dose - but don’t stop on your own.
What are the side effects for the baby?
Some newborns exposed to SSRIs in the third trimester may experience temporary symptoms like jitteriness, mild breathing trouble, or feeding difficulties - known as neonatal adaptation syndrome. This happens in about 30% of cases but almost always resolves within 2 weeks. There’s no evidence of long-term harm. The risk of persistent pulmonary hypertension (PPHN) is slightly higher (3-6 per 1,000 vs. 1-2 per 1,000), but still very rare.
Can I breastfeed while taking SSRIs?
Yes. Sertraline and paroxetine are considered the safest for breastfeeding because very little passes into breast milk. Fluoxetine can build up in the baby’s system and is usually avoided. Most experts agree that the benefits of breastfeeding and continued maternal mental health treatment outweigh any minimal infant exposure. Always monitor your baby for unusual sleepiness or feeding issues, but most infants show no effects.


Cole Newman
December 13, 2025 AT 19:45Look, I get it - everyone’s scared of meds during pregnancy. But let’s be real: if you’re crying in the shower every day and can’t even feed yourself, you’re not being ‘strong’ - you’re just suffering. SSRIs aren’t magic, but they’re the best tool we’ve got. Sertraline? Safe as milk. Paroxetine? Dump it. Stop letting fear drive your choices - data doesn’t lie.
Casey Mellish
December 14, 2025 AT 14:44As an Australian who’s seen both sides of the healthcare coin, I can tell you - this is one of those rare cases where the evidence is overwhelming. The WHO and RANZCOG both endorse SSRIs for moderate-to-severe perinatal depression. The risks of untreated illness? Far higher. Sertraline is the gold standard. Don’t let anecdotal horror stories override clinical consensus.
Emma Sbarge
December 15, 2025 AT 15:23Why is it always the American medical establishment pushing pills on women? In my grandma’s day, we toughed it out. We had community, we had church, we had each other. Now? We’re medicating away every emotional hiccup. This isn’t progress - it’s surrender. If your baby’s born with a little jitteriness, maybe that’s a sign you needed to slow down, not pop a pill.
Tommy Watson
December 17, 2025 AT 14:22ok so like i read this whole thing and i think the author is just a big pharma shill?? like who even wrote this? some phd who gets paid by zoloft? and what about that 28% autism stat? you just brushed it off like it’s nothing?? bruh. my cousin took lexapro and her kid still doesn’t talk at 4. coincidence? i think not.
Donna Hammond
December 18, 2025 AT 10:35Tommy, I hear you - but that cousin’s story isn’t the whole picture. The Lancet study controlled for genetics, family history, severity of depression - and found zero link to autism. The 28% figure? It’s from a study that didn’t adjust for maternal illness severity. When you do, the signal disappears. You’re not alone in your fear. But please, don’t let fear silence the science. Sertraline saved my life during my second pregnancy. I’m here to see my daughter graduate high school because I didn’t quit.
Richard Ayres
December 19, 2025 AT 01:28This is one of the most balanced, data-driven pieces I’ve read on perinatal mental health. The emphasis on absolute risk over relative risk is critical. Too many people fixate on the 80% increase in PPHN without realizing that’s still less than 1%. The real tragedy is women being told to stop their meds - and then being blamed when they relapse. This should be required reading for every OB-GYN.
Sheldon Bird
December 20, 2025 AT 11:17You’re not broken for needing help. You’re not selfish for taking care of yourself. And you’re definitely not weak for choosing to stay on sertraline. I’ve been there - postpartum anxiety so bad I couldn’t hold my baby without shaking. Meds didn’t make me a robot. They made me a mom. Keep going. You’ve got this. 💪❤️
Karen Mccullouch
December 21, 2025 AT 01:56Oh please. They’re just trying to normalize drugging pregnant women. What’s next? Add Ritalin for ‘baby brain’? The FDA doesn’t care about your baby - they care about profits. And don’t even get me started on how they bury the long-term data. You think your kid’s ‘fine’ now? Wait till they’re 16 and can’t leave the house. You’ll wish you’d just cried it out.
Ronan Lansbury
December 22, 2025 AT 16:30Interesting how the NIH ‘review’ conveniently ignores the 2019 Danish cohort study that showed a 22% increase in ASD among SSRI-exposed children. But of course - that study wasn’t funded by Pfizer. The data is suppressed. The pharmaceutical-industrial complex has turned pregnancy into a clinical trial. Wake up.
Harriet Wollaston
December 22, 2025 AT 16:35I was terrified to take anything during my first pregnancy. I cried for weeks. Then I started sertraline at 25mg. I slept. I ate. I smiled. My son is now 8 - brilliant, kind, athletic. No developmental delays. No anxiety. Just a happy kid with a mom who didn’t disappear into her depression. You’re not choosing drugs over your baby. You’re choosing yourself - so you can be there for them.
Lauren Scrima
December 23, 2025 AT 22:38So… you’re telling me the only way to be a ‘good mom’ is to be chemically calm? 🤔. Let me guess - the next article is ‘Why You Should Take Xanax for Toddler Tantrums.’ I mean, if you’re going to medicate your way through motherhood, why not just go full dystopia? At least admit it: we’re outsourcing emotional labor to Big Pharma.
sharon soila
December 24, 2025 AT 05:56Every human being deserves peace. Even during pregnancy. Even when it’s hard. Even when the world tells you to suffer in silence. Medicine is not a moral failing. It is a tool. And using it to protect your mind - so you can protect your child - is not weakness. It is wisdom. It is love. It is courage.
nina nakamura
December 24, 2025 AT 21:42Stop lying to women. The data is messy. The studies are funded by pharma. The risks are real. You think your kid’s fine now? Wait till they’re 12 and need therapy for anxiety you didn’t even know you gave them. You didn’t save your baby - you just delayed the consequences. And now you’re proud of it?
Constantine Vigderman
December 26, 2025 AT 02:27just wanna say thank you for this. i was about to quit my zoloft bc i was scared. now i’m gonna talk to my doc about staying on it. my baby deserves a mom who can breathe. and so do i. 🙏❤️