Sleep Apnea & Heart Risk Calculator
Your Risk Assessment
When you hear that sleep apnea can hurt your heart, it often sounds like a scare tactic. The reality is far more nuanced: untreated sleep apnea can directly impair the left ventricle, the chamber that pumps blood to the rest of your body. This article explains exactly how the breathing disorder fuels left ventricular dysfunction, what the latest research says, and how patients and clinicians can intervene before heart failure takes hold.
Key Takeaways
- Obstructive sleep apnea (OSA) triggers intermittent hypoxia, sympathetic surges, and negative intrathoracic pressure-all of which strain the left ventricle.
- Long‑term OSA increases the risk of reduced ejection fraction and overt heart failure by 30‑40% in middle‑aged adults.
- Polysomnography and bedside echocardiography are essential for detecting the combined impact of OSA and left ventricular dysfunction.
- Continuous Positive Airway Pressure (CPAP) therapy can improve ejection fraction by 5‑10% and lower hospital readmissions.
- A simple checklist-screen, diagnose, treat, monitor-helps clinicians protect cardiac function in patients with sleep‑related breathing disorders.
What Is Sleep Apnea?
Sleep Apnea is a sleep‑related breathing disorder characterized by repeated pauses in airflow during sleep. These pauses, called apneas, last at least 10 seconds and often recur dozens of times per hour. The two main types are:
- Obstructive Sleep Apnea (OSA): blockage of the upper airway despite ongoing respiratory effort.
- Central Sleep Apnea: a failure of the brain to send the signal to breathe.
OSA accounts for roughly 84% of all cases and affects an estimated 22 million American adults, with prevalence soaring to 50% in individuals with obesity or hypertension. Typical symptoms include loud snoring, witnessed pauses, morning headaches, and excessive daytime sleepiness. The condition is quantified using the apnea‑hypopnea index (AHI), where an AHI ≥15 events/hour qualifies as moderate‑to‑severe OSA.
Understanding Left Ventricular Dysfunction
Left Ventricular Dysfunction describes impaired pumping ability of the left ventricle, the heart’s primary workhorse. It is most commonly expressed as a reduced ejection fraction (EF)<50%, though diastolic dysfunction (preserved EF with impaired filling) is also clinically important.
Patients may experience fatigue, shortness of breath on exertion, orthopnea, or fluid buildup in the lungs. Left ventricular dysfunction is a core component of heart failure, a leading cause of hospitalization in adults over 65. Risk factors overlap heavily with sleep apnea: hypertension, obesity, diabetes, and coronary artery disease.
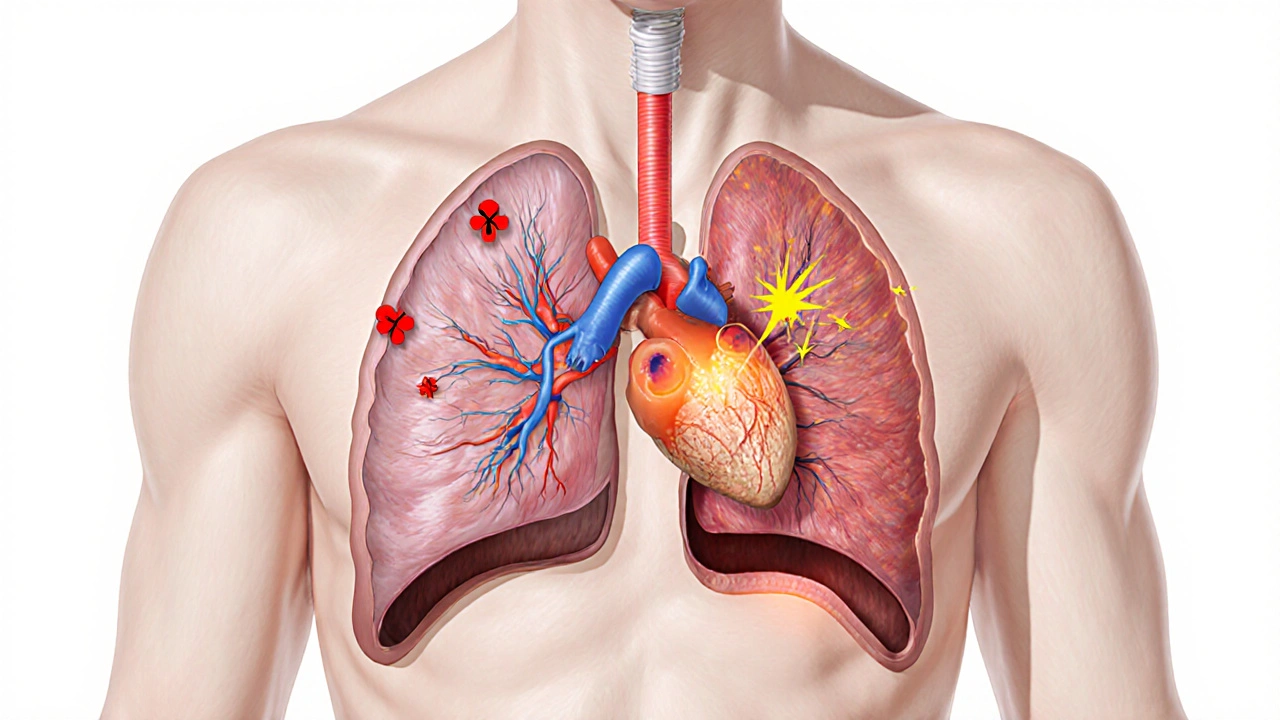
How Sleep Apnea Strains the Left Ventricle
The link between OSA and left ventricular dysfunction is not a simple one‑to‑one relationship; rather, several physiological pathways converge to burden the heart.
Intermittent Hypoxia and Oxidative Stress
Each apnea episode drops blood oxygen saturation, sometimes below 80%. This intermittent hypoxia provokes oxidative stress, damaging myocardial cells and promoting fibrosis. Studies using cardiac MRI have shown greater late gadolinium enhancement-an indicator of scar tissue-in OSA patients compared with matched controls.
Sympathetic Nervous System Activation
Repeated arousals trigger surge releases of norepinephrine and epinephrine. The resulting sympathetic overdrive raises heart rate and systemic vascular resistance, imposing a chronic afterload on the left ventricle. Over time, the ventricle remodels, becoming thicker and less compliant.
Negative Intrathoracic Pressure
During an obstructive event, the patient continues to inhale against a closed airway, generating negative pressures as low as -30cmH₂O. This suction not only pulls blood into the chest veins, increasing preload, but also stretches the myocardial wall, accelerating hypertrophy.
Inflammation and Endothelial Dysfunction
Elevated C‑reactive protein (CRP), interleukin‑6 (IL‑6), and tumor necrosis factor‑α (TNF‑α) have been documented in moderate‑to‑severe OSA. These inflammatory mediators impair endothelial nitric oxide production, fostering arterial stiffness and further elevating left ventricular afterload.
Clinical Evidence Linking OSA to Left Ventricular Dysfunction
Large‑scale cohort studies have quantified the risk. The 2022 Sleep‑Heart Health Study followed 5,800 adults for a median of 10years and reported a hazard ratio of 1.38 for developing left ventricular systolic dysfunction among those with AHI≥30, after adjusting for age, BMI, and hypertension.
Another prospective trial (n=1,200) compared untreated severe OSA patients with those who adhered to CPAP therapy for 12months. The CPAP group’s mean EF improved from 48%±6% to 55%±5%, while the untreated group showed a slight decline (48%→45%). Hospitalizations for heart failure dropped by 27% in the treated cohort.
These data reinforce that OSA is not merely a sleep nuisance-it is an independent predictor of left ventricular impairment.
Diagnosing Sleep Apnea in Patients With Left Ventricular Dysfunction
Because symptoms overlap, clinicians should maintain a high index of suspicion. Recommended steps:
- Screening questionnaires: Use the STOP‑BANG or Berlin tools during cardiac visits.
- Home sleep apnea testing (HSAT): For patients without significant comorbid lung disease, a Level3 HSAT can provide AHI data within a night.
- Polysomnography (PSG): Gold‑standard overnight study that captures airflow, effort, oxygen saturation, and EEG.
Polysomnography offers comprehensive recordings of respiratory events, sleep stages, and arousal indices, enabling precise classification of OSA severity.
- Echocardiography: Perform transthoracic echo to assess left ventricular ejection fraction, wall motion, and diastolic parameters.
Echocardiography is a non‑invasive ultrasound method that visualizes cardiac chambers, calculates EF, and detects subtle diastolic dysfunction.
Combining sleep study results with cardiac imaging offers a clear picture of how respiratory disturbances are impacting ventricular performance.
Managing Sleep Apnea to Protect the Heart
Therapeutic interventions target both the airway obstruction and the downstream cardiac effects.
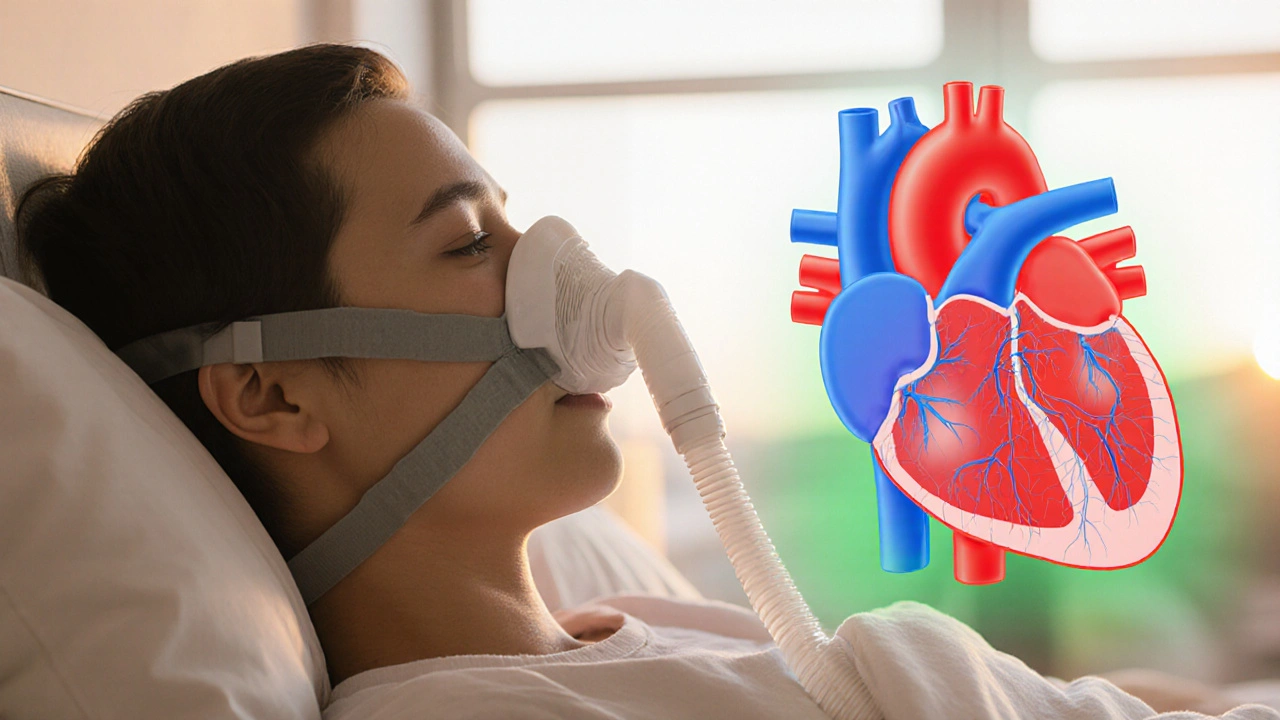
Continuous Positive Airway Pressure (CPAP)
Continuous Positive Airway Pressure (CPAP) delivers a constant stream of pressurized air through a mask, splinting the airway open throughout sleep. CPAP adherence of ≥4hours/night has been linked to:
- Improved EF by 5‑10% in moderate‑to‑severe OSA.
- Reduced nighttime systolic blood pressure by 6‑8mmHg.
- Lowered levels of CRP and IL‑6, indicating reduced systemic inflammation.
Lifestyle Modifications
Weight loss remains a cornerstone. A 10% reduction in body weight can lower AHI by up to 30%, easing cardiovascular strain. Regular aerobic exercise also attenuates sympathetic tone.
Adjunctive Therapies
Positional therapy (avoiding supine sleep), oral appliances, and upper airway surgery are options for patients intolerant of CPAP. In selected cases of central sleep apnea, adaptive servo‑ventilation (ASV) may be considered, though recent trials caution its use in advanced heart failure.
Impact of Treatment: A Comparative Snapshot
| Metric | Untreated OSA | CPAP‑Treated OSA |
|---|---|---|
| Ejection Fraction | 48%±6% | 55%±5% |
| NT‑proBNP (pg/mL) | 312±140 | 178±95 |
| Hospitalizations for Heart Failure | 0.32 per patient‑year | 0.23 per patient‑year |
| Mean Nighttime Systolic BP (mmHg) | 138±12 | 130±10 |
Practical Checklist for Clinicians and Patients
- Screen every patient with left ventricular dysfunction for OSA using STOP‑BANG.
- If SCORE ≥3, order a home sleep apnea test or refer for PSG.
- Obtain baseline echocardiogram before initiating CPAP.
- Educate patients on mask fitting, humidification, and the importance of ≥4hours/night use.
- Re‑evaluate EF, NT‑proBNP, and blood pressure at 3‑ and 12‑month intervals.
- Address modifiable risk factors: weight, alcohol, smoking, and sleep position.
Frequently Asked Questions
Can mild sleep apnea still affect heart function?
Yes. Even an AHI of 5-15 (mild OSA) can cause subtle nocturnal blood pressure spikes and increase sympathetic tone, which over many years may contribute to left ventricular remodeling.
How quickly can CPAP improve ejection fraction?
Most studies report measurable EF improvement within 3months of consistent CPAP use, with maximal gains appearing around 6-12months.
Is there a risk that CPAP could worsen heart failure?
In patients with preserved ejection fraction, CPAP is generally safe and beneficial. However, in rare cases of severe central sleep apnea with advanced systolic dysfunction, a different mode such as ASV may be needed.
Do weight‑loss surgeries help with OSA‑related heart problems?
Bariatric surgery can reduce AHI by 50‑70% and often leads to significant EF improvement, mainly by lowering afterload and systemic inflammation.
Should I get a sleep study if I already have a diagnosis of heart failure?
Absolutely. The prevalence of undiagnosed OSA in heart‑failure cohorts exceeds 40%. Identifying and treating OSA can reduce rehospitalizations and improve quality of life.


Nathan Squire
October 9, 2025 AT 20:28When considering the intricate relationship between obstructive sleep apnea and left ventricular dysfunction, one must first acknowledge the physiological cascade that bridges nocturnal breathing disturbances to chronic cardiac remodeling. Each apnea episode precipitates a sharp drop in arterial oxygen saturation, which in turn triggers a surge of sympathetic activity that persists well beyond the termination of the event. This sympathetic overdrive elevates heart rate and systemic vascular resistance, thereby imposing an intermittent pressure overload on the left ventricle. Simultaneously, the negative intrathoracic pressure generated during obstructive efforts increases left ventricular transmural pressure, further taxing myocardial fibers. Over weeks to months, these repeated insults foster myocardial hypertrophy, interstitial fibrosis, and a gradual reduction in ejection fraction. Empirical studies have quantified the risk, revealing a 30‑40 % increase in heart failure incidence among middle‑aged adults with untreated moderate‑to‑severe OSA. Importantly, the association remains robust after adjusting for confounders such as hypertension, obesity, and diabetes, underscoring a direct mechanistic link rather than mere comorbidity. Polysomnography, when paired with transthoracic echocardiography, provides the most definitive assessment of both respiratory disturbance severity and ventricular performance. Early identification allows clinicians to initiate continuous positive airway pressure therapy, which has been shown to improve left ventricular ejection fraction by roughly five to ten percentage points. Moreover, CPAP adherence correlates with reduced hospital readmissions for heart failure, translating into tangible cost savings for health systems. From a therapeutic standpoint, clinicians should adopt a checklist approach: screen high‑risk patients, confirm diagnosis with sleep study, prescribe CPAP, and schedule periodic cardiac imaging. Lifestyle modifications, such as weight loss and blood pressure control, synergize with device therapy to attenuate sympathetic drive. While some skeptics argue that CPAP benefits are merely a byproduct of improved sleep quality, randomized trials continuing beyond twelve months still demonstrate superior cardiac outcomes in the intervention arm. Therefore, dismissing OSA as a benign nuisance ignores a substantial body of evidence linking nightly hypoxia to progressive left ventricular dysfunction. In practice, the most harmful mistake is to treat the heart in isolation without addressing the underlying respiratory pathology. So, before you write off snoring as merely an annoyance, remember that the heart may be paying the ultimate price-sarcasm aside, the data are unequivocal.
satish kumar
October 18, 2025 AT 22:52It must be noted, however, that the purported causal link between sleep apnea and left ventricular dysfunction is, at best, a hypothesis rife with confounding variables; consequently, one should approach the literature with a healthy dose of skepticism, especially given the prevalence of selection bias in many cohort studies. Moreover, the dramatic improvements reported after CPAP initiation often coincide with simultaneous lifestyle interventions-weight loss, antihypertensive optimization, and increased physical activity-rendering attribution to airway therapy alone somewhat tenuous. While the authors of the original article present a tidy checklist, real‑world clinicians will readily admit that such protocols seldom translate seamlessly into practice; indeed, adherence rates hover around a discouraging 40 % in the general population, thereby limiting the external validity of the presented recommendations. In short, the narrative, though polished, may oversimplify a multifactorial dilemma.
Matthew Marshall
October 28, 2025 AT 00:16The heart dreads your snoring like a villain awaiting its cue. Yet, some claim the connection is mere hype-perhaps they’ve never felt a midnight gasp. Regardless, the drama of a silent night is worth the preventive effort.
Lexi Benson
November 6, 2025 AT 02:40Wow, another groundbreaking revelation that breathing at night matters-shocking, right? Your body will thank you, or it will file a grievance, but either way, the advice stands. :)
Vera REA
November 15, 2025 AT 05:04Sleep apnea contributes to intermittent hypoxia, which elevates sympathetic tone and imposes hemodynamic stress on the left ventricle. Studies consistently show a dose‑response relationship between apnea‑hypopnea index severity and reductions in ejection fraction. Early detection via polysomnography combined with echocardiographic screening allows timely initiation of CPAP, mitigating progressive remodeling. Cultural awareness of sleep health can improve screening uptake across diverse populations.
John Moore
November 24, 2025 AT 07:28I agree with the earlier point that practical steps matter more than rhetorical flair; implementing CPAP alongside lifestyle changes offers the most balanced approach. Let’s keep the focus on evidence‑based interventions rather than sarcasm.
Adam Craddock
December 3, 2025 AT 09:52Current guideline recommendations from the American Heart Association emphasize that patients with moderate to severe obstructive sleep apnea should undergo baseline cardiac imaging, regardless of symptomatic status. Furthermore, longitudinal follow‑up at six‑month intervals is advised to monitor ejection fraction trends and adjust therapeutic strategies accordingly. The integration of sleep specialists into cardiology clinics has shown to streamline care pathways and improve adherence to both CPAP and pharmacologic regimens.
Kimberly Dierkhising
December 12, 2025 AT 12:16From a hemodynamic standpoint, the repeated cyclic hypoxemic insults precipitate baroreflex-mediated catecholamine surges, augmenting afterload and precipitating concentric hypertrophy of the left ventricle. The resultant diastolic dysfunction is often quantified via tissue Doppler imaging, revealing reduced E′ velocities concomitant with elevated E/E′ ratios. Pathophysiologically, oxidative stress pathways upregulate matrix metalloproteinases, facilitating extracellular matrix remodeling and fibrosis. Therapeutic modulation with CPAP attenuates these maladaptive cascades, as evidenced by reductions in NT‑proBNP and improved strain parameters.
Alexia Rozendo
December 21, 2025 AT 14:40You’ve hit the nail on the head with the technical jargon-nothing like a good dose of cardiology speak to keep us awake at night. Still, the takeaway is crystal clear: treating the airway can reverse the molecular mess you just described. Kudos for breaking it down in terms even the rest of us can tolerate.
Kimberly Newell
December 30, 2025 AT 17:04hey folks, just wanted to drop a quick tip-if u think you snore like a chainsaw, get a sleep study ASAP. u might be surprised how much your heart thanks u for it. stay chill.
Drew Burgy
January 8, 2026 AT 19:28Of course the pharma companies love to keep us in the dark about the real power of CPAP; they’d rather push pills than let us breathe easy. I’ve read the hidden files that show how a simple mask can cut heart failure rates dramatically, yet the mainstream media stays silent. So, while they’re busy selling you another beta‑blocker, remember that the real fix might just be a piece of plastic humming at night-no strings attached, unless you count the wires.