When you take more than one medication, your body doesn’t treat them like separate guests at a party. It processes them all together-and sometimes, one drug can mess with how another one moves through your system. This is called a pharmacokinetic drug interaction. It doesn’t mean the drugs fight each other. Instead, one changes how your body absorbs, distributes, metabolizes, or gets rid of the other. And that can lead to side effects, reduced effectiveness, or even serious harm.
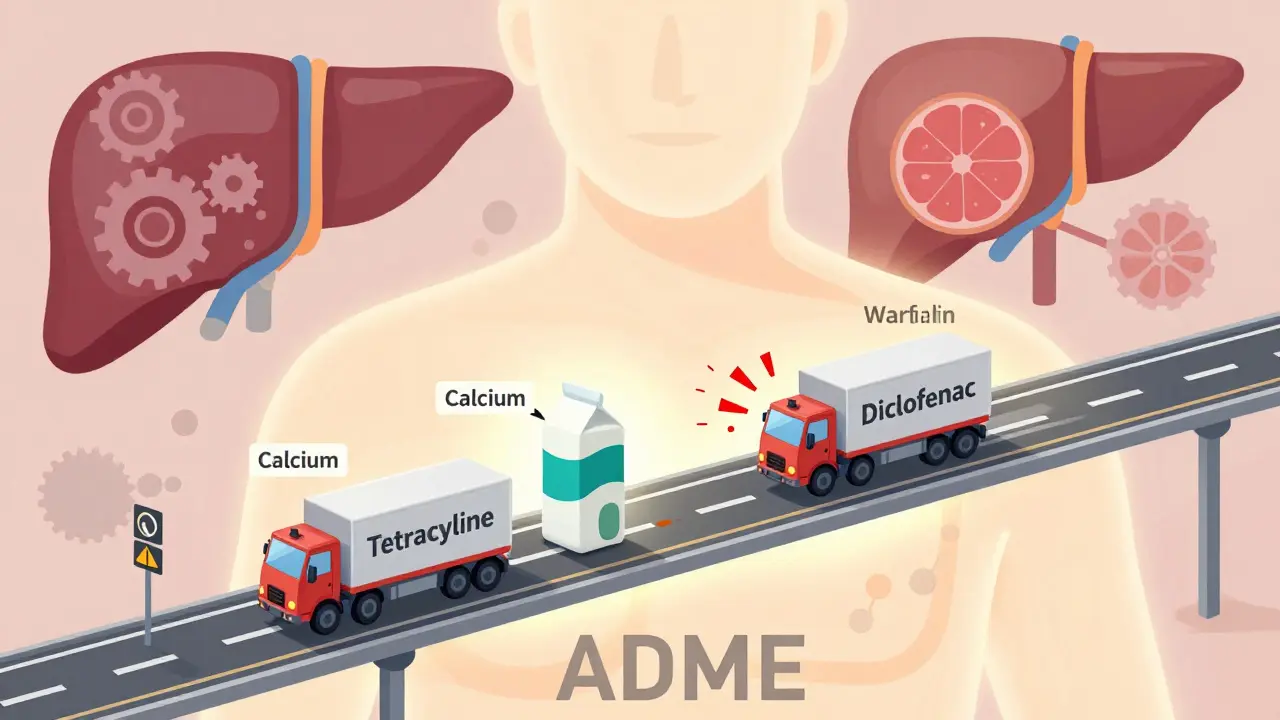
How Your Body Moves Drugs Around (ADME)
Your body handles every drug the same way: it absorbs it, distributes it, metabolizes it, and excretes it. These four steps are called ADME. If one drug interferes with any of them, it changes how much of the other drug actually reaches your bloodstream or stays in your system.
For example, if you take an antacid for heartburn and then take a thyroid medication like levothyroxine right after, the antacid can block the thyroid drug from being absorbed. That means your thyroid treatment won’t work as well. The fix? Space them out by at least 4 hours. Simple, but most people don’t know this.
Absorption: When Drugs Block Each Other’s Entry
Not all drugs enter your bloodstream the same way. Some need stomach acid to be absorbed. Others get stuck if they meet certain foods or minerals.
Tetracycline antibiotics, used for infections, are a classic case. If you take them with milk, yogurt, or calcium supplements, the calcium binds to the antibiotic in your gut. This stops it from being absorbed-up to half of the dose disappears. Same thing with iron supplements and tea or coffee. The tannins in those drinks bind to iron and reduce absorption.
Even opioids can slow down how fast other drugs move through your gut. Morphine, for instance, reduces stomach movement, which delays how quickly acetaminophen (Tylenol) gets into your blood. It might not sound serious, but if you’re counting on pain relief, this delay matters.
Distribution: When Drugs Compete for Space in Your Blood
Once drugs get into your bloodstream, they mostly stick to proteins like albumin. But there’s only so much room. If two drugs want to bind to the same protein, one can push the other off.
This happens with warfarin (a blood thinner) and diclofenac (an NSAID painkiller). When diclofenac is added, it kicks warfarin off the protein. Suddenly, more free warfarin is floating around. Since only the free form works, your blood thins more than expected. That raises your risk of bleeding-sometimes dangerously.
But here’s the catch: this kind of interaction doesn’t always cause problems. Your liver often responds by breaking down the extra free drug. So unless the drug has a very narrow safety window-like warfarin, digoxin, or phenytoin-it usually doesn’t lead to harm.
Metabolism: The Most Dangerous Interactions Happen Here
This is where things get serious. Most drugs are broken down in your liver by enzymes called cytochrome P450 (CYP). The most important ones are CYP3A4 and CYP2D6. If one drug blocks or speeds up these enzymes, it changes how fast another drug is cleared from your body.
Let’s say you take metoprolol (a beta-blocker) and propafenone (an anti-arrhythmic). Propafenone blocks CYP2D6, the enzyme that breaks down metoprolol. That means metoprolol builds up in your blood. Your heart rate might drop too low. Doctors have to reduce the metoprolol dose when both are used together.
Now think about grapefruit juice. Just one glass can block CYP3A4 for a whole day. That means if you’re taking simvastatin (a statin for cholesterol), your body can’t break it down. Levels spike, and your risk of muscle damage goes up. The FDA says over 85 prescription drugs interact with grapefruit juice. If you take any of them, skip the grapefruit.
On the flip side, some drugs speed up metabolism. St. John’s Wort, a popular herbal supplement for mood, can turn on CYP3A4 and CYP2D6. If you’re on birth control, an antidepressant, or a transplant drug like cyclosporine, St. John’s Wort can make them work poorly. You might get pregnant. Or reject your new organ. Or feel worse than before.
Excretion: When Kidneys Get Overloaded
Your kidneys are the main way your body flushes out drugs. But if two drugs use the same pathway, they can block each other.
Probenecid, used for gout, blocks the kidney’s ability to get rid of penicillin and other antibiotics. That’s actually useful in hospitals-it helps keep antibiotics in the body longer. But if you’re not in a hospital and you take probenecid with a common NSAID like ibuprofen, you could end up with too much of the antibiotic in your blood. That raises the risk of side effects.
Even worse: methotrexate (used for cancer and autoimmune diseases) can build up to dangerous levels if taken with NSAIDs. The result? Bone marrow damage, kidney failure, or even death.
P-glycoprotein (P-gp) is another key player. It’s like a pump that pushes drugs out of your kidney and gut cells. If a drug blocks P-gp, other drugs pile up. Itraconazole (an antifungal) blocks P-gp, which means digoxin (used for heart rhythm) stays in your body longer. Digoxin levels can double. That can trigger dangerous heart rhythms. The FDA says about 1 in 5 serious drug interactions involve transporter proteins like P-gp.
Real-Life Examples: What Can Go Wrong
An 85-year-old woman was taking venlafaxine (an antidepressant) and propafenone (a heart rhythm drug). Both are processed by CYP2D6 and blocked by P-gp. Together, they caused venlafaxine levels to spike. She started seeing things that weren’t there-hallucinations-and became agitated. She ended up in the hospital.
Another case: an older man on phenobarbital (for seizures) started taking lamotrigine (another seizure drug). Phenobarbital sped up the metabolism of lamotrigine, creating toxic byproducts. He developed low white blood cells and low platelets-signs of bone marrow failure. He needed emergency treatment.
The Institute for Safe Medication Practices says warfarin, insulin, and digoxin are the top three drugs involved in serious interaction-related ER visits. They account for over one-third of all cases.
How to Protect Yourself
You don’t need to be a scientist to avoid these problems. Here’s what actually works:
- Keep a full list of everything you take. That includes prescriptions, over-the-counter meds, vitamins, and herbal supplements. A 2020 study found that people who kept a written list reduced interaction risks by 47%.
- Use one pharmacy. Pharmacists have software that checks for interactions across all your meds. In the U.S., this prevents about 150,000 bad reactions every year.
- Ask your doctor or pharmacist: "Could this interact with my other meds?" and "Are there foods or drinks I should avoid?" Research from Mayo Clinic shows asking these two questions improves detection by 63%.
- Space out problematic pairs. If you take calcium or iron with thyroid meds, wait at least 4 hours. Same with antibiotics and dairy.
- Avoid grapefruit juice entirely if you take any prescription drug. The FDA lists 85+ drugs that react with it. It’s not worth the risk.
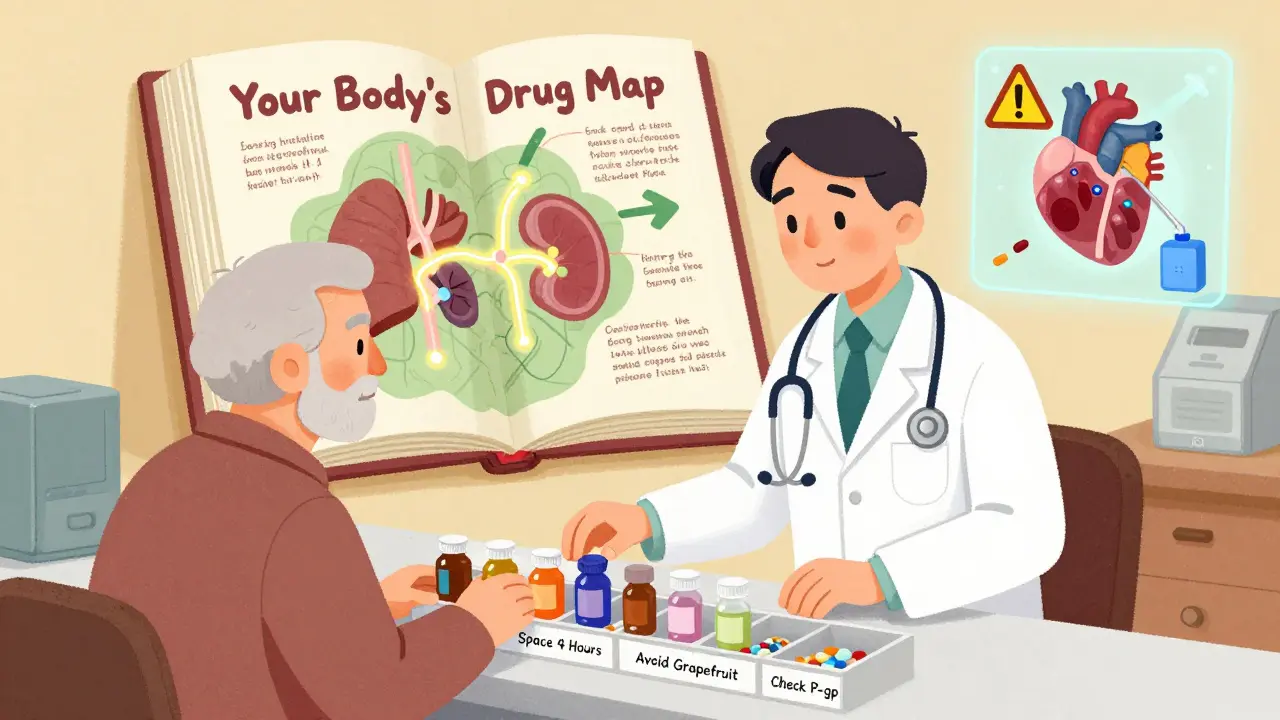
What Doctors and Pharmacists Do
Hospitals and clinics now use electronic systems that warn doctors about potential interactions. One study found these alerts catch 85% of major risks. But here’s the problem: doctors get so many alerts that they ignore nearly half of them. That’s called alert fatigue.
Pharmacists are the real heroes here. When they review your meds-especially if you’re on five or more drugs-they catch problems doctors miss. A 2019 Medicare study showed pharmacist-led reviews cut adverse events by 22%. In the U.S., pharmacists prevent over 1.2 million serious interactions every year.
The Future: Personalized Medicine
Scientists are now looking at your genes. Some people are "poor metabolizers" of certain drugs because of their CYP2C19 or CYP2D6 genes. That means even normal doses can be too much. The FDA now includes pharmacogenomic info on 340 drug labels. In the next few years, genetic testing before prescribing could cut interaction-related hospital stays by 30%.
Telehealth apps are also catching up. By 2023, 78% of major U.S. health systems had built-in interaction checkers in their patient portals. You’ll soon be able to scan your meds and get instant alerts.
One thing won’t change: you’re still your own best defense. Stay informed. Stay curious. And never assume your meds are safe just because they were prescribed.
What’s the difference between pharmacokinetic and pharmacodynamic drug interactions?
Pharmacokinetic interactions are about how your body moves the drug-absorption, distribution, metabolism, or excretion. Pharmacodynamic interactions are about how the drugs affect your body together. For example, taking two sedatives might make you extra drowsy because both act on the same brain receptors. One changes your body’s handling of the drug; the other changes the drug’s effect.
Can herbal supplements cause pharmacokinetic interactions?
Yes. St. John’s Wort is one of the most common offenders. It boosts liver enzymes that break down many drugs, including birth control, antidepressants, and transplant meds. Garlic, ginkgo, and green tea can also interfere with blood thinners. Even though they’re "natural," they’re not risk-free. Always tell your pharmacist about supplements.
Why is grapefruit juice so dangerous with medications?
Grapefruit juice blocks the CYP3A4 enzyme in your gut, which is responsible for breaking down many drugs before they enter your bloodstream. This means more of the drug gets absorbed than intended. A single glass can last 24 hours. Even if you take your medication hours after the juice, the enzyme is still blocked. That’s why the FDA warns against grapefruit with over 85 medications.
Do all drug interactions cause obvious symptoms?
No. Some interactions build up slowly. You might feel fine at first, but over days or weeks, drug levels rise and side effects appear. For example, digoxin toxicity can cause fatigue, nausea, or blurry vision-symptoms easily mistaken for aging. That’s why regular check-ups and medication reviews are crucial.
Can aging increase my risk of drug interactions?
Yes. As you get older, your liver and kidneys don’t work as well. About 40% of adults over 65 have reduced kidney function. That means drugs stay in your body longer. Older adults also take more medications-on average, five or more. The combination of slower processing and more drugs raises interaction risk significantly. The American Geriatrics Society specifically lists 13 medications to avoid in older adults because of this.
What to Do Next
Start today. Grab your medication list. Write down everything-even the aspirin you take once a week. Take it to your next doctor or pharmacist appointment. Ask them to check for interactions. If you’re on warfarin, digoxin, or insulin, make this a priority. Don’t wait until something goes wrong. Your safety isn’t something to guess about. It’s something you can control-with the right information.


Chelsea Cook
February 9, 2026 AT 17:10So let me get this straight - grapefruit juice is basically the toxic ex of your medication cabinet? 🍊💀 I drank half a gallon last week with my statin. Guess I’m scheduling my next ER visit. Thanks, science.
Jacob den Hollander
February 11, 2026 AT 04:45Wow, this was so helpful… I didn’t realize my morning coffee was basically sabotaging my iron pills. I’ve been taking them together for years. Oof. I’m gonna start spacing them out now. Thanks for the heads-up! Also, I think I just spelled ‘levothyroxine’ wrong. Again. Sorry.
Brandon Osborne
February 12, 2026 AT 10:34YOU’RE ALL JUST IGNORING THE REAL ISSUE HERE. THE PHARMA COMPANIES KNOW ABOUT THESE INTERACTIONS AND THEY DON’T CARE. THEY’RE MAKING BILLIONS WHILE WE’RE DYING IN OUR BEDS FROM ‘ACCIDENTAL’ TOXICITY. WHY ISN’T THIS ON THE NEWS? WHY AREN’T WE PROTESTING? THIS IS A CRIME AGAINST HUMANITY. I’M NOT JUST A PATIENT - I’M A VICTIM. AND I’M NOT SILENT ANYMORE.
Marie Fontaine
February 12, 2026 AT 23:26Yessss! I’ve been telling my grandma this for months 😊 She takes 8 meds and grapefruit every morning. I just sent her this article. She said ‘Oh honey, I thought that was just a myth like the one about carrots giving you night vision.’ Now she’s switching to orange juice. Progress!
Ken Cooper
February 14, 2026 AT 05:46so like… i always thought drug interactions were just a thing you read about in textbooks. turns out my weird headache after taking ibuprofen with my antibiotic wasnt just ‘bad luck’? i mean… wow. i’ve been taking amoxicillin with my morning yogurt for 3 years. that’s wild. maybe i should’ve asked my pharmacist. i just assumed they knew. guess not.
MANI V
February 16, 2026 AT 03:34People like you who treat medicine like a buffet are the reason our healthcare system is collapsing. You think a 4-hour gap solves everything? You’re just delaying the inevitable. Your body is a temple, and you’re treating it like a vending machine. You don’t get to pick and choose which chemicals to mix. This isn’t a game. You’re playing with your life.
Susan Kwan
February 17, 2026 AT 19:51Wow. A post that doesn’t sound like it was written by an AI trying to win a Pulitzer. Finally. Someone who gets it. Also, St. John’s Wort is not a ‘natural mood booster’ - it’s a sneaky little saboteur. I knew a guy who got pregnant on birth control because he ‘trusted’ herbal stuff. Don’t be that guy.
Random Guy
February 19, 2026 AT 01:52so like… i took my blood pressure med with grapefruit juice once. just once. and then i had this weird dream where my heart was singing opera. i woke up crying. i don’t know if it was the drug or the juice or if my soul just… left. i’m never doing it again. also i think my dog hates me now.
Ryan Vargas
February 19, 2026 AT 05:33What we’re witnessing here isn’t just pharmacokinetic interaction - it’s a systemic collapse of epistemological trust in biomedical authority. The human body, as a dynamic, self-regulating system, has evolved over millennia to process xenobiotics, yet we’ve outsourced our physiological autonomy to a pharmaceutical-industrial complex that profits from pharmacological chaos. The CYP450 enzymes aren’t merely metabolic tools - they’re the last bastion of biological sovereignty. When we introduce grapefruit juice into this sacred equilibrium, we’re not just altering drug half-lives - we’re eroding the ontological integrity of homeostasis itself. And yet, the FDA’s warnings are merely band-aids on a hemorrhaging system. The real solution? A return to ancestral dietary patterns, fasting, and the rejection of synthetic molecules altogether. Or, at the very least, a citizen-led pharmacovigilance network.
Tasha Lake
February 20, 2026 AT 06:39From a clinical pharmacology standpoint, the inhibition of CYP3A4 by furanocoumarins in grapefruit is a textbook example of first-pass metabolism disruption. The AUC of simvastatin can increase up to 15-fold, and the risk of rhabdomyolysis spikes exponentially. What’s more concerning is that P-gp inhibition compounds this effect. We’re not talking about ‘maybe’ - we’re talking about a pharmacokinetic perfect storm. And yet, 78% of patients still don’t know this. That’s a public health failure.
Brett Pouser
February 21, 2026 AT 10:40My mom’s on like 12 meds and she swears by her ‘herbal tea blend’ - turns out it had garlic and ginkgo in it. She almost bled out during a dental cleaning. Now she only drinks chamomile. I’m proud of her. Also, I just told my cousin to stop taking his OTC painkiller with his blood thinner. He said ‘But it’s just Advil.’ I said ‘Yeah, and Advil is also a tiny bomb.’ He got it. Small wins.
Tom Forwood
February 22, 2026 AT 10:44so i work at a pharmacy and let me tell you - we catch like 30 of these a week. people come in with 7 different bottles and say ‘is this okay?’ and we’re like ‘oh god no.’ one guy took his thyroid med with his calcium supplement and then asked why he was still tired. we had to explain that it’s like putting a key in a lock and then gluing the lock shut. he said ‘ohhhhhhh.’ that’s why i love this job. we’re basically drug detectives.
John McDonald
February 24, 2026 AT 05:19Good post. Really well-structured. I’m a nurse and I’ve seen too many ER visits from people who didn’t know about grapefruit or spacing out meds. The fact that pharmacists prevent 1.2 million interactions a year? That’s the real MVP. We need more of them. Also, I’m gonna start asking my patients: ‘What’s in your supplement drawer?’ That’s gonna be my new mantra.