When you fill a prescription for a generic drug-say, metformin for diabetes or lisinopril for high blood pressure-you might assume the insurance company pays a small, straightforward amount. But here’s the truth: what insurance actually pays for generics isn’t what you see on your receipt, and it’s not even what the pharmacy gets paid. The real cost is buried in layers of contracts, hidden fees, and financial incentives that rarely benefit you or your plan.
Generics don’t work like brand-name drugs
Brand-name drugs often come with big rebates. Manufacturers pay pharmacy benefit managers (PBMs) hundreds of millions in kickbacks to get their drugs listed on insurance formularies. These rebates can be 30% to 70% of the list price. That’s why you’ll see a brand-name drug with a $200 list price, but your insurer only pays $60 after the rebate. It looks like a win. But generics? They don’t play that game. There’s no rebate system worth talking about. Why? Because there are 20 companies making the exact same pill. Competition drives the price down to pennies. A 100-pill bottle of generic atorvastatin might cost $4 at the pharmacy. If a manufacturer tried to offer a 20% rebate on that, it’d be 8 cents. Not worth the paperwork. So instead of rebates, PBMs use something else: spread pricing.Spread pricing: the hidden tax on generics
Here’s how it works. Your insurer thinks it’s paying $8.50 for that $4 generic. The pharmacy is told to accept $4. The PBM pockets the $4.50 difference. That’s spread pricing. It’s not a rebate. It’s not a discount. It’s a profit margin hidden inside your insurance plan. You won’t see this on your explanation of benefits. You won’t see it on your pharmacy receipt. But it’s real. In 2022, the U.S. Department of Health and Human Services found the average spread on generic prescriptions was $4.73 per fill. Multiply that by millions of fills a year, and you’re talking billions in hidden profits. Employers who self-insure are especially affected. One Fortune 500 company discovered their PBM was charging $8.50 per generic while paying pharmacies only $4.25. They had no idea. No disclosure. No audit rights. Just a line item on a monthly bill they assumed was fair.Why PBMs don’t want you to use generics
It sounds backwards, but PBMs often have a financial reason to avoid generics. If a brand-name drug has a 60% rebate, and a generic has no rebate at all, the PBM makes more money steering you toward the brand. That’s not a typo. Rightway Healthcare documented cases where PBMs excluded a $0.15-per-dose generic in favor of a $5-per-dose brand-name drug with a 60% rebate. Even after the rebate, the net cost was higher. But the PBM’s profit? It went up. The patient paid more. The insurer paid more. Everyone lost-except the PBM. This isn’t rare. A 2023 Commonwealth Fund report found PBMs design formularies to favor high-rebate drugs-even when lower-cost generics are available. They’re not optimizing for your health or your wallet. They’re optimizing for their bottom line.
What insurance really pays for generics
Let’s break it down with real numbers:- Wholesale Acquisition Cost (WAC): $4.00 (what the pharmacy pays the manufacturer)
- Pharmacy reimbursement: $4.00 (what the pharmacy gets paid by the PBM)
- Insurer payment: $8.50 (what your plan is billed)
- PBM profit (spread): $4.50
- Your copay: $3.00 (if you have one)
Why transparency is almost impossible
Most insurance plans don’t know what they’re really paying. PBMs hide the true cost of generics in complex contracts. Even large employers with legal teams struggle to audit their PBM agreements. A 2023 survey by the National Business Group on Health found 68% of large employers couldn’t determine the actual net cost of generic drugs. Why? Because contracts are written in legalese. Terms like “administrative fee,” “dispensing fee,” and “network discount” mask the spread. You’re not just paying for the drug-you’re paying for a middleman’s profit, and you don’t know how much. And when you ask for details? PBMs say, “It’s proprietary.”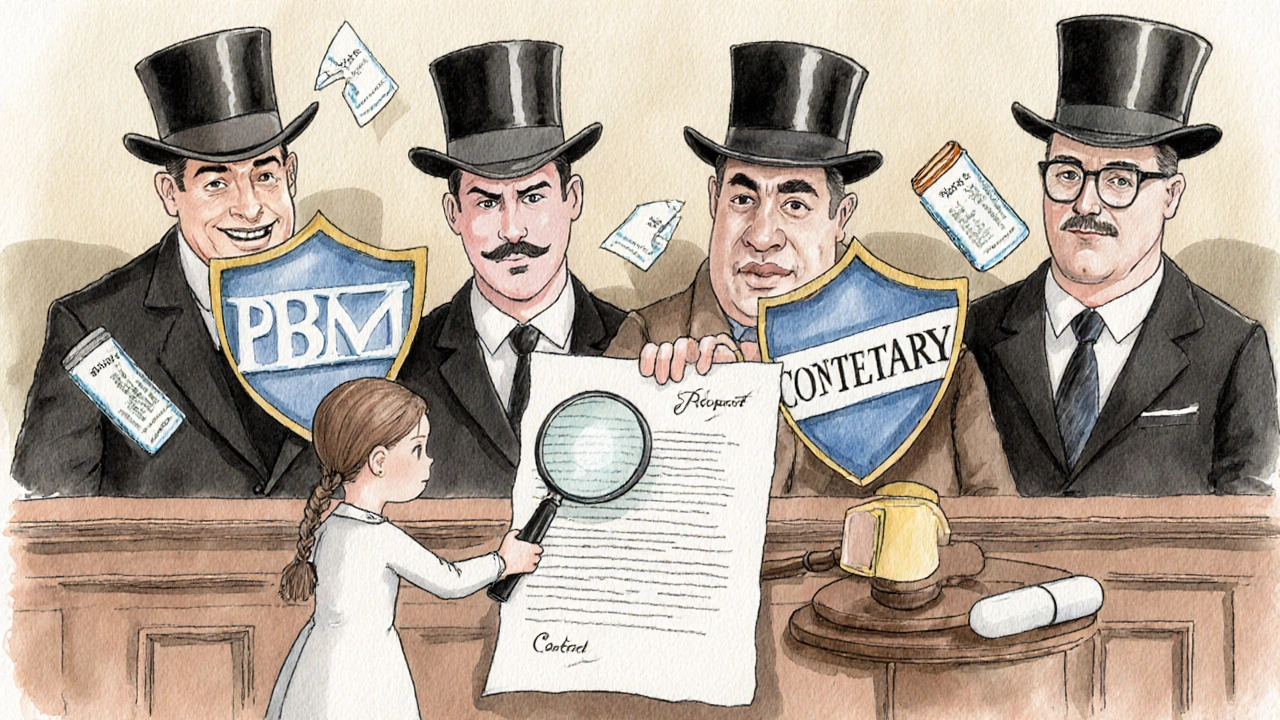
What’s changing-and what’s not
There’s pressure to fix this. The No Surprises Act of 2020 started requiring some transparency. The Biden administration’s 2024 executive order asked HHS to examine practices that limit generic use. And in 2024, 42% of large employers moved to pass-through pricing-where PBMs charge a flat fee instead of keeping the spread. But change is slow. The three biggest PBMs-CVS Caremark, Express Scripts, and OptumRx-control 80% of the market. They have no incentive to make things simple. In fact, they’ve spent millions lobbying against transparency laws. Meanwhile, the Inflation Reduction Act of 2022 explicitly excluded generics from Medicare drug price negotiation. Why? Because lawmakers assumed competition already keeps prices low. But that ignores the PBM middleman. The real problem isn’t the manufacturer’s price-it’s what gets added on top.What you can do
If you’re an individual with private insurance, your power is limited. But if you’re on an employer plan-or you’re an employer yourself-there are steps:- Ask your benefits provider: “Do you use spread pricing on generics?”
- Request a full audit of your PBM contract. Look for terms like “administrative fee,” “network discount,” or “rebate pass-through.”
- Push for pass-through pricing. That means your plan pays the pharmacy’s actual cost plus a fixed fee-no hidden cuts.
- Use tools like GoodRx or SingleCare to compare cash prices. Sometimes paying cash is cheaper than using insurance.
The bottom line
Generics are supposed to save money. And they do-when the system works. But the rebate model that works for brand-name drugs doesn’t apply here. Instead, PBMs profit from opacity. What insurance pays for generics isn’t the price on the bottle. It’s not even what the pharmacy receives. It’s what the PBM decides to charge-and keep. The system isn’t broken. It’s working exactly as designed-for the middlemen, not for patients or payers. Until transparency becomes law, the real cost of your generic prescription will stay hidden. And you’ll keep paying for it-without knowing how much.Do generic drugs have rebates like brand-name drugs?
No, generic drugs rarely have rebates. Unlike brand-name drugs, which have high list prices and complex rebate deals with pharmacy benefit managers (PBMs), generics are already priced low due to competition. Manufacturers don’t offer meaningful rebates because there’s no room to cut prices further without losing money. Instead, PBMs profit from spread pricing-keeping the difference between what insurers pay and what pharmacies get paid.
Why does my insurance pay more for a generic than the pharmacy receives?
This happens because of spread pricing. Your insurer is billed a higher amount than what the pharmacy is paid. The difference-often $3 to $5 per prescription-is kept by the pharmacy benefit manager (PBM) as profit. For example, if the pharmacy gets $4 for a generic and your insurer is charged $8.50, the PBM pockets $4.50. This is rarely disclosed on your statements, making it hard to track.
Can PBMs block generic drugs to favor brand-name ones?
Yes. PBMs sometimes exclude low-cost generics from formularies if the brand-name version offers a large rebate. Even if the generic is cheaper overall, the PBM makes more money by steering patients toward the brand-name drug with a 60% rebate. This creates a perverse incentive: the system rewards higher spending, not lower costs. The Commonwealth Fund and Rightway Healthcare have documented multiple cases of this happening.
How can I find out what my insurance really pays for generics?
If you’re covered under an employer plan, ask your HR or benefits team for a PBM contract audit. Look for spread pricing or hidden administrative fees. If you’re an individual, compare your copay to cash prices on apps like GoodRx. If the cash price is lower, your insurance is likely overpaying due to spread pricing. Transparency laws are coming, but for now, you need to ask the hard questions.
Is there a move toward more transparent generic drug pricing?
Yes. In 2024, 42% of large employers switched to pass-through pricing, where PBMs charge a flat fee instead of keeping the spread. The Biden administration’s 2024 executive order directed HHS to examine practices that limit generic use. Legislation in several states now requires PBM disclosure of generic acquisition costs. By 2026, federal rules may require full transparency. But change is slow-PBMs still control 80% of the market and resist reforms that cut their profits.


Clay Johnson
November 28, 2025 AT 12:19Generics are the ultimate economic paradox. They exist to reduce cost, yet the system inflates them into profit engines. The real tragedy isn't the spread pricing-it's that we've normalized it. We accept opacity as part of the deal, like paying for air. But air isn't owned by middlemen. Neither should our prescriptions be.
Transparency isn't a policy change. It's a moral baseline.
Jermaine Jordan
November 29, 2025 AT 15:06THIS IS A NATIONAL SCANDAL. We're being robbed in plain sight, and no one's screaming. PBMs aren't intermediaries-they're parasites. They take a $4 pill and bill $8.50. And we call this healthcare? This isn't capitalism. This is feudalism with a pharmacy receipt.
Someone needs to sue these companies into oblivion. Not regulate. Not investigate. SUE.
Chetan Chauhan
November 29, 2025 AT 16:18u mean the pmb? i think its pbs? or is it pbs? anyway yeah generics r cheap but u know what? my friend got metformin for 2$ cash at walmart so why even use ins? lol
Pranab Daulagupu
November 30, 2025 AT 23:13Spread pricing is a structural flaw in the PBM ecosystem. The incentive misalignment is pathological: profit is derived from disparity, not efficiency. The solution isn't just transparency-it's structural reform. Pass-through models are the only ethical framework left. We must institutionalize them before the system collapses under its own weight.
Barbara McClelland
December 1, 2025 AT 13:05Y’all need to check GoodRx before you swipe your card. I used to pay $12 for my lisinopril until I found out the cash price was $3.50. My pharmacist was like, ‘Yeah, your insurance is getting gouged.’ I felt so dumb.
Don’t assume your plan is working for you. Ask. Push. Compare. You’ve got more power than you think.
Alexander Levin
December 2, 2025 AT 12:05pbms are just the tip of the iceberg. 👁️👁️ next they'll start charging you for breathing. #BigPharma #ShadowGovernment
Ady Young
December 4, 2025 AT 02:46Barbara’s right-GoodRx is a game-changer. I’ve been using it for my dad’s blood pressure med. Cash price is half what his insurance billed. And honestly? I’m not mad at the pharmacy. They’re just following the script.
The real villains are the ones hiding behind ‘administrative fees’ and ‘proprietary contracts.’ We need to stop treating this like a black box and start treating it like a public service.
Travis Freeman
December 5, 2025 AT 04:17Just want to say-this thread is so important. I’m from a small town in Mississippi, and my mom’s on 5 generics. She didn’t know she was being overcharged until I showed her GoodRx. Now she pays $2.50 out of pocket. No copay. No insurance hassle.
It’s not just about money. It’s about dignity. Everyone deserves to know what they’re paying for-and not be tricked into paying more for less.
Keep speaking up. This stuff matters.