Multiple System Atrophy (MSA) is not Parkinson’s disease. Even though it looks like it at first-slowness, stiffness, shaky movements-it’s something far more aggressive and far less responsive to treatment. If you or someone you know has been told they have MSA, especially the parkinsonian type (MSA-P), it’s critical to understand what you’re really dealing with: a fast-moving, multi-system brain failure that doesn’t follow the rules of more common movement disorders.
What Makes MSA-P Different from Parkinson’s?
MSA-P stands for Multiple System Atrophy with predominant parkinsonism. About 65 to 70% of MSA cases fall into this category. The symptoms? Slowness of movement, stiff muscles, trouble with balance, and sometimes tremors. Sounds familiar? It should. But here’s where it breaks down: the tremors in MSA-P aren’t the classic resting tremor you see in Parkinson’s. They’re jerky, irregular, and often appear when the person is trying to hold a position-not when they’re at rest.And then there’s the response to levodopa, the gold-standard Parkinson’s drug. In Parkinson’s, levodopa can dramatically improve movement for years. In MSA-P? Only 15 to 30% of patients get any benefit at all-and even then, it fades within a year or two. That’s not a minor difference. It’s a diagnostic red flag. If someone with parkinsonism doesn’t respond to levodopa after a few months of high-dose trials, MSA should be on the shortlist.
Another key clue? The face. People with MSA-P often develop a mask-like expression, not from emotional withdrawal, but because the muscles controlling facial movement are stiff and unresponsive. Their voice becomes quiet, breathy, or strained. Swallowing gets harder. Chewing becomes a chore. These aren’t late-stage signs. They can show up within the first year.
The Silent Killer: Autonomic Failure
That’s not the worst part. The real danger in MSA isn’t just movement-it’s the body’s automatic systems shutting down. Autonomic dysfunction is the hallmark of MSA, and it’s often the first sign, appearing years before tremors or stiffness.Nearly everyone with MSA-P develops orthostatic hypotension-a dangerous drop in blood pressure when standing. This isn’t just dizziness. It’s fainting, falls, head injuries, and sometimes sudden cardiac events. Studies show 90% of MSA patients have this condition, with blood pressure plunging 30 mmHg or more within minutes of standing. It’s why so many patients end up wearing compression stockings, drinking salt water, and taking medications like midodrine or droxidopa just to stay upright.
Bladder control? Gone in 85 to 90% of cases. Urinary urgency, incontinence, retention-it’s relentless. Men face near-universal erectile dysfunction, often as the earliest symptom. Sleep? Almost everyone has REM sleep behavior disorder, where they act out dreams-kicking, yelling, even falling out of bed. Sleep apnea adds another layer of risk, reducing oxygen levels overnight and straining the heart.
And then there’s temperature control. Half of patients lose the ability to sweat in specific areas. One leg might sweat normally, the other doesn’t. The back is cold, the face is flushed. This isn’t just discomfort-it’s a sign the brainstem, the body’s thermostat, is failing.
How Fast Does It Progress?
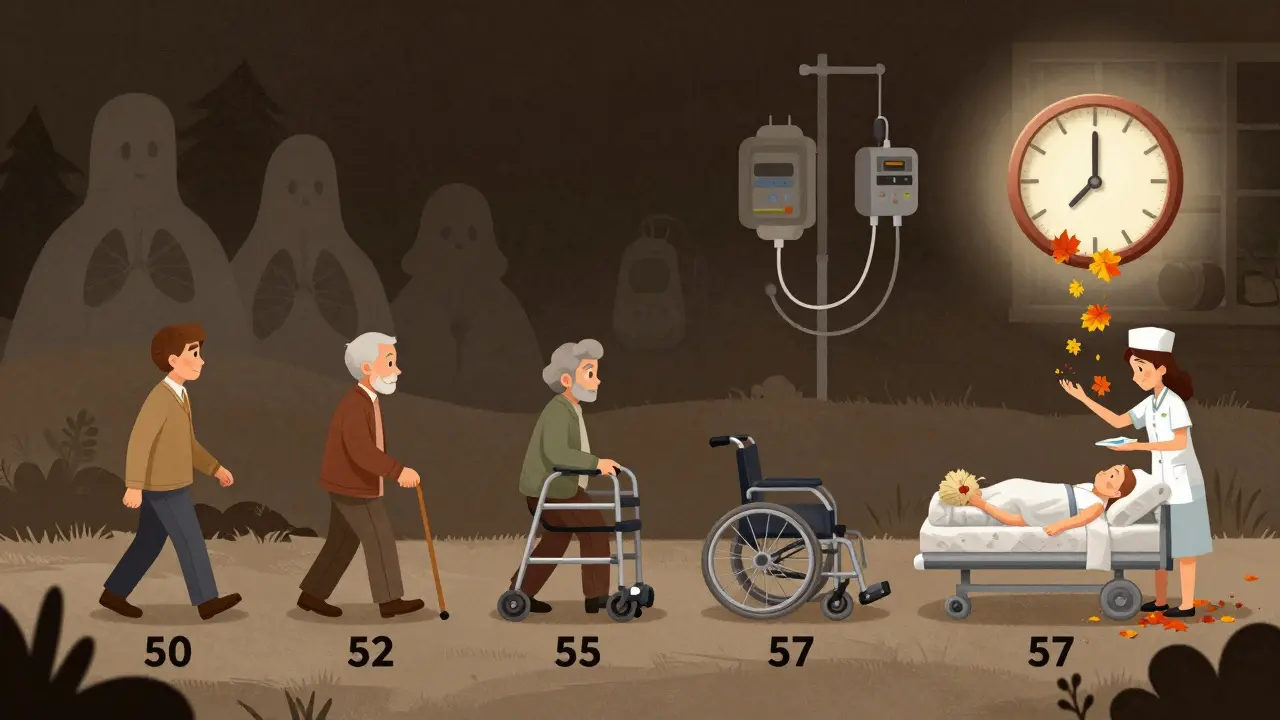
MSA-P doesn’t wait. Unlike Parkinson’s, which can take decades to severely limit mobility, MSA-P moves fast. Within 1 to 2 years, 85% of patients have had at least one fall. By 3.5 years, most need a cane or walker. By 5.3 years, they’re in a wheelchair. Within 5 years, half have lost nearly all their motor function.The numbers are brutal. Median survival from symptom onset is 6 to 10 years. Only 9 to 23% of patients are alive 10 years after diagnosis. The most common causes of death? Aspiration pneumonia from swallowing problems (15%), respiratory infections (45%), and sudden cardiac arrest (20%).
There’s a cruel irony here: the better someone responds to levodopa, the longer they tend to live. Those with no response have a median survival of 6.2 years. Those with even partial improvement? Around 9.8 years. But even then, it’s not a cure-it’s just a slight delay in the inevitable.
Why Diagnosis Takes So Long
Doctors miss it. Early MSA-P is easily mistaken for Parkinson’s. Even neurologists can be fooled. The difference? Timing. In Parkinson’s, autonomic symptoms appear late-often after 10 years. In MSA, they’re there within the first year, sometimes before movement problems even start. That’s the key. If someone has dizziness, urinary issues, and erectile dysfunction before they start shuffling, it’s not Parkinson’s. It’s MSA.Imaging helps. An MRI might show the “hot cross bun” sign-a distinctive pattern in the brainstem seen in about half of MSA-C cases, and sometimes in MSA-P. Putaminal atrophy, or shrinkage of a deep brain structure, is another red flag. But even with imaging, diagnosis isn’t certain until 3 to 5 years after symptoms begin. By then, the damage is already widespread.
Researchers are trying to fix this. A new biomarker panel combining blood tests (neurofilament light chain levels, which spike in MSA), detailed MRI scans, and autonomic function tests aims to cut diagnosis time to under a year. Results from a major study are expected in mid-2024. But until then, the diagnosis remains a race against time.
What Treatments Actually Work?
There is no cure. No drug stops MSA from progressing. No therapy reverses the damage. Everything is about managing symptoms and trying to keep people safe and comfortable as long as possible.For low blood pressure: midodrine, droxidopa, fludrocortisone. For bladder issues: catheters, anticholinergics, or Botox injections. For sleep disorders: melatonin or clonazepam. For speech and swallowing: speech therapy with swallow assessments and dietary changes. Physical therapy helps maintain mobility, but it won’t slow the disease.
Levodopa is still tried-usually at high doses (up to 1,000 mg/day) for 3 to 6 months. But doctors warn patients upfront: don’t expect miracles. If there’s no improvement in 6 months, stop. It’s not worth the side effects.
And there’s no hope on the horizon yet. Clinical trials targeting alpha-synuclein-the abnormal protein that clumps in MSA brains-have failed. The most promising trial in 2023 showed only a 1.2-point slowdown on a rating scale over 18 months. That’s statistically tiny and clinically meaningless.
As of late 2023, there are only three active global trials trying to modify the disease. The MSA Coalition says we’re decades behind Parkinson’s research. The reason? It’s rare. Fewer than 50,000 people in the U.S. have it. Drug companies don’t see the profit. Patients don’t get the attention.
Living with MSA-P: The Human Cost
It’s not just physical. A 2021 survey of 327 MSA patients found that 78% rated their quality of life as “poor” or “very poor” within just four years of diagnosis. Compare that to Parkinson’s, where only 35% feel that way at the same stage. The isolation, the loss of independence, the fear of choking or falling alone-these are the invisible wounds.One patient, diagnosed at 52, wrote on a support forum: “By 18 months, I needed a cane. By three years, a walker. By four, a wheelchair.” Another, 55, said: “My neurologist said most of us don’t live past eight years. That’s not a prognosis-it’s a countdown.”
There’s no sugarcoating this. MSA-P steals your body, your dignity, and your time. It doesn’t ask for permission. It doesn’t wait for you to be ready.
What Comes Next?
Early diagnosis is the only real advantage we have. If you’re a caregiver or a patient with unexplained dizziness, urinary problems, or voice changes-especially if you’re over 50-push for a full autonomic workup. Don’t settle for “it’s just aging.” Don’t accept “maybe Parkinson’s.” Ask: Could this be MSA?Start multidisciplinary care now. A neurologist, a urologist, a speech therapist, a physical therapist, a palliative care specialist. These aren’t optional. They’re lifelines. A swallow study can prevent pneumonia. A catheter schedule can prevent infections. A wheelchair can prevent a fatal fall.
And if you’re reading this because you’re facing this diagnosis? You’re not alone. But you’re in a fight with a disease that doesn’t care about hope. Your job now isn’t to find a cure. It’s to plan for the next 6 to 10 years-with clarity, with support, and with as much control as you can hold onto.
Is Multiple System Atrophy the same as Parkinson’s disease?
No. While MSA-P shares symptoms like slowness and stiffness with Parkinson’s, it’s a different disease. MSA affects more areas of the brain, including those controlling blood pressure, bladder, and breathing. It progresses faster, responds poorly to levodopa, and includes severe autonomic failure early on-something Parkinson’s doesn’t do until much later.
How long do people live after being diagnosed with MSA-P?
Median survival is 6 to 10 years from the start of symptoms. About half of patients lose most motor function within 5 years. Only 9 to 23% survive 10 years after diagnosis. Survival is shorter for those who don’t respond to levodopa.
Can MSA be cured or stopped with medication?
No. There is no cure, and no medication slows or stops the progression of MSA. Treatments focus on managing symptoms-like low blood pressure, bladder issues, and sleep problems-but they don’t change the course of the disease.
Why is MSA-P so hard to diagnose early?
Early symptoms like dizziness, urinary problems, or voice changes mimic other conditions, including Parkinson’s. Autonomic symptoms often appear before movement issues, but doctors don’t always connect them. Accurate diagnosis usually takes 3 to 5 years, by which time significant brain damage has already occurred.
What are the most common causes of death in MSA-P?
The top causes are respiratory infections (45%), sudden cardiac death (20%), and aspiration pneumonia from swallowing difficulties (15%). These are all linked to the autonomic and motor decline caused by MSA.
Are there any new treatments or clinical trials for MSA?
As of late 2023, there are only three active global clinical trials targeting disease modification. Most recent trials, including those targeting alpha-synuclein, have shown minimal or no benefit. Research is focused on early biomarkers-like blood tests and advanced MRI-to improve diagnosis speed, not yet on effective therapies.


Abby Polhill
December 25, 2025 AT 02:10MSA-P is essentially a neurodegenerative cascade where the brainstem and basal ganglia just... stop coordinating. The autonomic failure isn't a side effect-it's the core pathology. The fact that levodopa barely touches it tells you this isn't dopaminergic degeneration alone. It's alpha-synuclein glomming onto oligodendrocytes, forming glial cytoplasmic inclusions, and wrecking myelin integrity across multiple systems. That's why MRI shows putaminal atrophy and the hot cross bun sign-those aren't incidental, they're diagnostic anchors. The disease is a perfect storm of motor, autonomic, and respiratory network collapse, and we're still treating it like a Parkinson's variant when it's its own beast.
Most neurologists don't get this until it's too late because the DSM and ICD codes still lump it under 'parkinsonism.' We need a paradigm shift in how we classify synucleinopathies-not by motor phenotype, but by anatomical spread and cellular tropism.
Delilah Rose
December 25, 2025 AT 06:52I remember when my dad was first diagnosed with what they thought was Parkinson’s at 61. He had dizziness, urinary retention, and a voice that sounded like it was underwater-none of which his neurologist connected to movement issues. By the time they did the MRI and saw the putaminal atrophy, he’d already fallen three times. It took 14 months to get the right diagnosis. By then, he was on midodrine, a catheter, and a wheelchair. The worst part wasn’t the physical decline-it was how quickly people stopped visiting. No one knows what to say when someone’s dying from a disease they’ve never heard of. I wish more doctors would stop waiting for tremors to show up. If someone over 50 has unexplained orthostatic hypotension and bladder issues, run the MSA panel before prescribing Sinemet. It’s not just about treatment-it’s about preparing families for the speed of the decline. I’ve seen too many people waste months chasing the wrong diagnosis while their body burns out.
And yes, the survival stats are brutal. But knowing what you’re facing? That’s the only thing that lets you plan. We got him a voice amplifier, a swallow study, a hospice consult-all before he could no longer speak. It wasn’t hopeful, but it was honest. And that mattered more than any drug ever could.
Bret Freeman
December 25, 2025 AT 10:47Let me be clear-this isn’t just a rare disease. It’s a systemic failure of medical research. We pour billions into Parkinson’s because it’s profitable, but MSA? It’s a graveyard for patients and a dead end for pharma. You’re telling me we can’t find a cure for a disease that kills people in 6 to 10 years because there are only 50,000 cases in the US? That’s not science-that’s capitalism with a stethoscope. And don’t get me started on how doctors dismiss autonomic symptoms as ‘aging’ or ‘stress.’ My cousin was told she had anxiety because she passed out standing up. She was 58. Three years later, she’s in a hospice bed, choking on her own saliva. This isn’t a medical mystery. It’s a moral one. We let people die slowly because their disease doesn’t make money. And we call ourselves healers.
Austin LeBlanc
December 27, 2025 AT 05:51Why do people keep saying ‘it’s not Parkinson’s’ like that’s supposed to comfort someone? It’s not a reassurance-it’s a death sentence with better branding. MSA isn’t just worse-it’s crueler. Parkinson’s lets you live a decade with dignity. MSA steals your bladder, your voice, your breath, and your dignity before you even lose your legs. And then we tell families to ‘focus on quality of life’ like that’s some kind of silver lining. What quality? The kind where you need a catheter to pee and a feeding tube to swallow? The kind where your husband can’t hold your hand because his muscles are frozen? Don’t sugarcoat this. It’s a slow-motion murder by biology. And the fact that we’re still running placebo trials instead of aggressive research? That’s not negligence. That’s complicity.
niharika hardikar
December 28, 2025 AT 18:50It is imperative to recognize that the diagnostic delay in Multiple System Atrophy is not merely a clinical oversight but a structural deficiency in neurologic education and resource allocation. The presence of early autonomic dysfunction, particularly orthostatic hypotension and urogenital dysautonomia, must be prioritized in differential diagnosis protocols for parkinsonian syndromes. Current diagnostic criteria, while scientifically sound, remain inaccessible to primary care providers due to lack of standardized screening tools and insufficient training in autonomic testing. The proposed biomarker panel incorporating neurofilament light chain and quantitative MRI metrics represents a promising avenue; however, its implementation requires cross-institutional collaboration and funding from governmental health agencies, not solely private pharmaceutical interests. The global burden of MSA, though numerically small, demands equitable access to diagnostic infrastructure, particularly in low-resource settings where symptom attribution to ‘aging’ remains pervasive and lethal.
John Pearce CP
December 30, 2025 AT 09:42It is regrettable that the medical establishment continues to underfund research into rare neurodegenerative disorders. The United States, as the world’s leading innovator in biomedical science, has a moral obligation to prioritize diseases that disproportionately affect its aging population. MSA, with its rapid progression and devastating autonomic consequences, represents a critical gap in our neuroprotective strategy. The failure of alpha-synuclein-targeted therapies underscores the necessity for alternative approaches-epigenetic modulation, mitochondrial stabilization, and glial cell reprogramming. We must redirect funding from redundant clinical trials toward high-risk, high-reward platforms. Moreover, diagnostic protocols must be standardized across all VA and Medicare facilities. To allow patients to suffer for years under misdiagnosis is not only medically indefensible-it is a betrayal of the American promise of compassionate care.
EMMANUEL EMEKAOGBOR
December 31, 2025 AT 08:37As a physician from Nigeria, I have seen MSA cases in our urban centers, though they are often misclassified as Parkinson’s due to limited access to MRI and autonomic testing. The core issue is not only biological but systemic: in low-income countries, the absence of neurologists and diagnostic tools means patients are left without even the palliative options described here. I applaud the emphasis on multidisciplinary care, but we must also advocate for global equity in neurology. A patient in Lagos should have the same chance at a swallow study or a catheter schedule as one in Boston. MSA does not discriminate by geography-why should our care? Let us not wait for profit-driven trials to fix this. Let us build networks, train community health workers, and share protocols. Knowledge is the only treatment we can distribute freely.
Jillian Angus
January 1, 2026 AT 11:12Pankaj Chaudhary IPS
January 2, 2026 AT 15:10As a medical professional with over two decades of experience in neurology, I wish to emphasize that the management of MSA-P requires a proactive, multidisciplinary, and patient-centered approach from the moment of suspected diagnosis. Early intervention with autonomic stabilization-through fluid and salt loading, compression garments, and pharmacologic agents like droxidopa-is not merely supportive; it is life-preserving. The integration of speech-language pathology for dysphagia risk mitigation, urological management for neurogenic bladder, and palliative care consultation must be initiated concurrently with diagnosis, not as afterthoughts. Furthermore, caregiver education and psychological support are not ancillary-they are central to sustaining quality of life. While a cure remains elusive, the architecture of compassionate, anticipatory care can transform the trajectory of this disease from one of unmitigated decline to one of dignified stewardship. Let us not wait for breakthroughs to begin caring. We already have the tools. We need only the will.