Methadone vs. Buprenorphine Decision Tool
This interactive tool helps you understand which opioid treatment medication—methadone or buprenorphine—might be more appropriate for your specific situation based on your health profile and opioid use history. Remember: This is not medical advice. Always consult with your doctor for personalized treatment decisions.
Your Situation
When someone is trying to recover from opioid addiction, medication can be a lifeline. Methadone and buprenorphine are two of the most trusted tools in this fight. They don’t just reduce cravings-they help people get back to work, reconnect with family, and stay alive. But they’re not without their downsides. The side effects can be heavy, confusing, and sometimes scary. Knowing what to expect isn’t about scaring people off-it’s about making sure they stay in treatment.
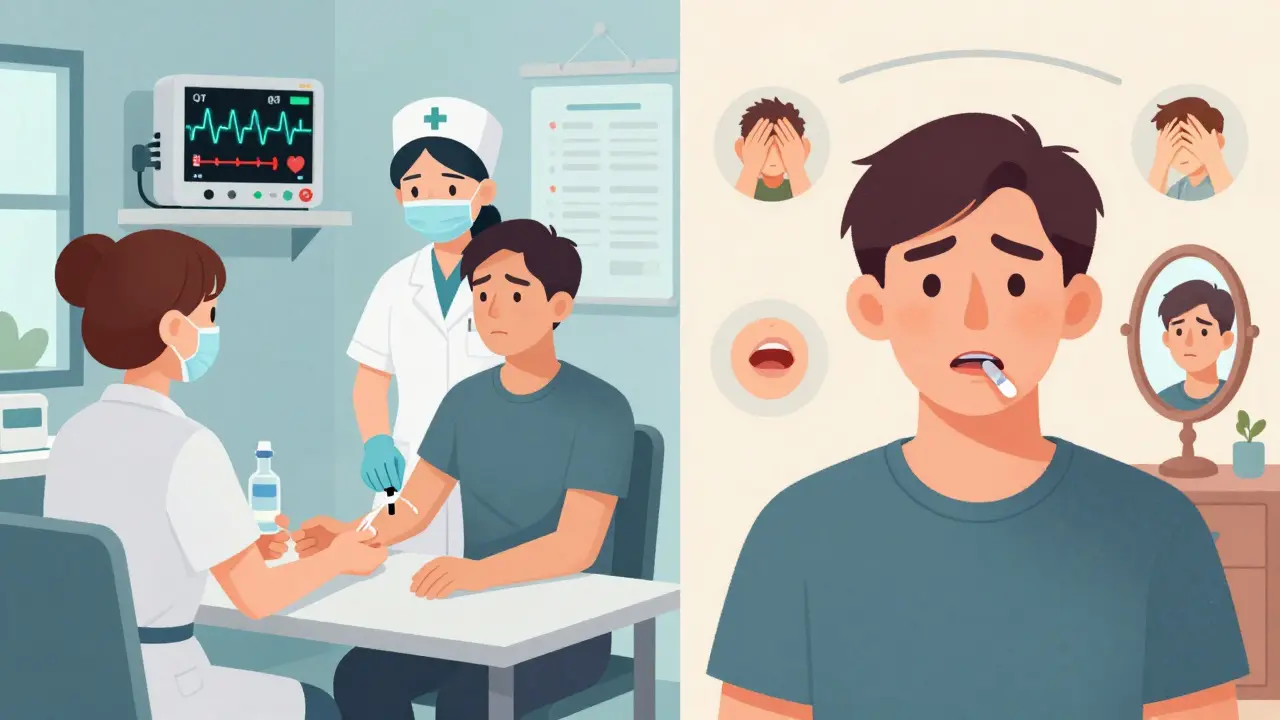
What Methadone Does to Your Body
Methadone is a full opioid agonist. That means it fully activates the same brain receptors as heroin or fentanyl, but without the high. It’s long-lasting, often working for 24 to 36 hours. That’s why people on methadone usually only need one dose a day. But that strength comes with risks.
Constipation is one of the most common complaints. Around 25 to 40% of people on methadone say they need laxatives just to go to the bathroom. It’s not just uncomfortable-it can lead to serious bowel issues if ignored. Nausea and vomiting affect up to one in three people, especially in the first few weeks. Sleepiness hits hard, too. Many users describe feeling "like a zombie," unable to focus at work or drive safely. One Reddit user wrote: "I stopped methadone because I couldn’t stay awake during my shift. I lost my job."
The biggest danger with methadone is its effect on the heart. It can stretch the QT interval on an EKG, which increases the risk of dangerous heart rhythms. At doses over 100mg a day, this happens in up to 35% of users. That’s why doctors recommend a baseline heart test before starting and regular checkups after. People with existing heart conditions or those taking other meds like antidepressants or antibiotics are at higher risk.
Sexual side effects are often left out of the conversation. About 30% of long-term methadone users report trouble getting or keeping an erection. Libido drops. For some, it’s a quiet, isolating burden that keeps them from talking to their doctor. And then there’s the risk of overdose-especially in the first weeks. Methadone builds up slowly in the body, so if someone takes too much too fast, they can stop breathing. That’s why methadone is only given in clinics at first, with daily supervision.
What Buprenorphine Does to Your Body
Buprenorphine is different. It’s a partial agonist. Think of it like turning a faucet halfway on instead of all the way. It reduces cravings and withdrawal, but it doesn’t produce the same intense high-or the same level of danger. That’s why it’s safer for home use and why it’s become the most prescribed medication for opioid addiction in the U.S.
The most common side effect? Mouth problems. Because it’s taken as a tablet or film that dissolves under the tongue, many people get numbness, tingling, or soreness in their mouth. Up to 35% report this. If you swallow it instead of letting it dissolve, you lose most of the dose. Some users say it tastes awful, like metal or plastic, and that makes sticking with it harder.
Headaches are another big one. Around 30 to 40% of buprenorphine users get them, sometimes daily. They’re usually mild, but they can be persistent enough to make people quit. Nausea still happens, but less than with methadone-closer to 20%. Constipation is also less common, affecting about 25% of users.
But here’s the catch: buprenorphine has a ceiling. After a certain dose-usually around 16 to 24mg-it stops working better. For someone with high opioid tolerance, especially after years of fentanyl use, that ceiling can feel like a wall. They might still feel cravings, still feel the urge to use. One user on Healthgrades wrote: "Suboxone helped me stop shooting up, but I still felt like I needed more. I ended up using on the side."
There’s also the risk of withdrawal if you take it too soon after using other opioids. If you’re still under the influence of heroin or oxycodone when you take buprenorphine, it can kick out those drugs from the receptors and trigger sudden, severe withdrawal. That’s called precipitated withdrawal. It happens in 15 to 25% of first-time users and can be so intense that people leave treatment before they even get started.
Which One Is Safer?
Safety isn’t just about overdose risk-it’s about what happens over time.
Methadone has a higher risk of fatal overdose, especially in the first month. Studies show it’s 2.5 times more likely than buprenorphine. But here’s the twist: people who stick with methadone are more likely to stay in treatment. One 2024 study found that 81.5% of methadone users were still in care after two years. For buprenorphine? Only about 11% stayed that long. That’s not because buprenorphine doesn’t work-it’s because many people feel it doesn’t work enough.
Buprenorphine is safer for the heart. It doesn’t stretch the QT interval the way methadone does. It’s also less likely to cause respiratory depression. That’s why it’s often recommended for people who live alone, have other health issues, or use alcohol or benzodiazepines. But if you’re someone who’s been using high doses of opioids for years, buprenorphine might not be strong enough.
And then there’s the mental side. Both meds can make it harder to focus. But studies show methadone users have worse memory and attention problems-especially when it comes to driving. One 2007 study found methadone users performed 25 to 30% worse on visual memory tests than buprenorphine users. That’s not just inconvenient-it’s dangerous.
What the Experts Say
There’s no one-size-fits-all answer. Dr. Nora Volkow from NIDA says methadone is more effective, but only if you can manage the risks. Dr. Keith Ahmad from Canada says buprenorphine should be first-line for most people because it’s safer and more accessible. Dr. John Renner from Boston says methadone is still the gold standard for people with severe, long-term addiction-especially those who’ve used fentanyl.
And the data backs them up. People with fentanyl use disorder are more likely to be put on methadone because it handles high tolerance better. Meanwhile, buprenorphine is more common for newer users, people with jobs, or those who need flexibility.
But access matters. Since 2023, any doctor can prescribe buprenorphine-no special waiver needed. That’s good. But a 2024 study found that 43% of primary care doctors don’t know how to start someone on it safely. That means people might get the wrong dose, or be put on it too soon, triggering withdrawal. Meanwhile, methadone clinics are still limited, especially in rural areas. You might need to drive hours for your daily dose.

What You Can Do About the Side Effects
Side effects don’t have to be permanent. Many fade after a few weeks as your body adjusts. But there are things you can do to make them easier.
- For constipation: Drink more water, eat fiber, move your body. If that doesn’t work, ask for a stool softener or laxative. Don’t suffer in silence.
- For drowsiness: Don’t drive or operate heavy machinery until you know how the med affects you. Most people find their energy returns after 4 to 6 weeks.
- For mouth issues (buprenorphine): Let the film or tablet dissolve completely. Don’t chew it. Don’t eat or drink for 15 minutes after. Rinse your mouth with water afterward.
- For headaches: Try over-the-counter pain relievers like acetaminophen. Avoid ibuprofen if you’re on methadone-it can affect liver enzymes.
- For heart concerns: If you’re on methadone and your dose is over 100mg, ask for an EKG. If you feel your heart racing, dizzy, or faint, get checked immediately.
- For sexual side effects: Talk to your provider. There are treatments. You’re not alone.
And never mix these meds with alcohol, benzodiazepines, sleep aids, or other opioids. That’s when overdoses happen. Even if you’ve been on one of these meds for months, adding another depressant can shut down your breathing.
What Comes Next?
New forms of buprenorphine are coming. There’s a monthly injection (Sublocade) and a six-month implant (Probuphine). They avoid mouth issues and daily dosing-but they can cause pain or swelling at the injection or implant site. About half of users report discomfort there.
Methadone is also being improved. New versions in clinical trials aim to reduce heart risks without losing effectiveness. And doctors are starting to use genetic tests to see how fast your body processes methadone. Some people break it down fast and need higher doses. Others break it down slow and get side effects even on low doses.
But the bottom line hasn’t changed: both methadone and buprenorphine save lives. The side effects are real-but so is the relief they bring. People on these meds are more likely to stay alive, hold a job, and rebuild relationships. The goal isn’t to be perfect. It’s to be stable.
If you’re struggling with side effects, talk to your provider. Don’t quit because it’s hard. Adjustments can be made. Doses can be changed. Support is there. You don’t have to suffer alone.
Can you overdose on methadone or buprenorphine?
Yes, but the risk is very different. Methadone can cause overdose, especially during the first few weeks or if taken with alcohol or benzodiazepines. It’s responsible for about 30% of prescription opioid overdose deaths in the U.S. Buprenorphine has a ceiling effect-after a certain dose, it doesn’t increase respiratory depression. That makes fatal overdose much less likely, even with higher doses. Still, combining it with other depressants can be deadly.
Which one is better for someone with a heart condition?
Buprenorphine is generally safer. Methadone can cause QT prolongation, which increases the risk of dangerous heart rhythms. People with existing heart problems, a history of arrhythmias, or those taking other medications that affect the heart are at higher risk on methadone. A baseline EKG is recommended before starting methadone, especially at doses above 100mg per day. Buprenorphine doesn’t carry that same cardiac risk, making it the preferred choice for many with heart conditions.
Why do some people still use opioids while on buprenorphine?
Buprenorphine has a ceiling effect. For people with very high opioid tolerance-especially those who’ve used fentanyl regularly-it may not fully block cravings or withdrawal. If the dose is too low (under 16mg), or if the person’s tolerance is extremely high, they might still feel the urge to use. That’s why some need methadone instead. It’s stronger and doesn’t have that ceiling. It’s not a failure-it’s a sign that the treatment needs adjusting.
Can you switch from methadone to buprenorphine?
Yes, but it’s not simple. You need to be off methadone for several days and fully in withdrawal before starting buprenorphine. If you start too soon, you can get sudden, severe withdrawal. Most providers recommend reducing methadone to 30mg or less per day, then waiting 48 to 72 hours before switching. This process should always be done under medical supervision. Some people switch successfully. Others find they need to stay on methadone because buprenorphine doesn’t control their symptoms well enough.
How long do side effects last?
Most side effects improve within 2 to 6 weeks as your body adjusts. Constipation, drowsiness, and nausea usually get better. Headaches and mouth discomfort from buprenorphine may linger longer but often become manageable. Sexual side effects and cognitive issues can take months to improve-and sometimes don’t fully go away. That doesn’t mean you should quit. Many people find the trade-off is worth it: better sleep, no cravings, no withdrawal, and the ability to function normally. Talk to your provider about long-term side effects. There are often solutions.
Are there alternatives to methadone and buprenorphine?
There’s naltrexone, which blocks opioids entirely and comes as a daily pill or monthly injection (Vivitrol). But it doesn’t reduce cravings or withdrawal, so you have to be fully detoxed before starting-often requiring a 7- to 10-day stay in a detox center. It’s not as effective as methadone or buprenorphine for most people, especially those with severe addiction. It’s more common for people who’ve already stabilized and want to prevent relapse. For active opioid use disorder, methadone and buprenorphine remain the most effective options.
If you’re considering treatment, don’t let fear of side effects stop you. The goal isn’t to feel perfect-it’s to feel stable. And for millions of people, that’s exactly what these medications deliver.


Holly Robin
February 1, 2026 AT 04:20So let me get this straight-we’re giving people FULL OPIOIDS to fix opioid addiction?? And we wonder why the overdose crisis keeps growing?? This isn’t treatment, it’s just swapping one drug for another with a doctor’s stamp on it. Methadone clinics are just government-approved heroin dens. And don’t even get me started on how they monitor you like a prisoner. They don’t care if you live or die-they just want to keep the funding flowing. #BigPharmaLies
Lily Steele
February 2, 2026 AT 18:13I’ve been on buprenorphine for 18 months. The mouth numbness sucked at first, but I got used to it. Headaches faded after a month. I’m working full-time, seeing my kids again, and actually sleeping through the night. It’s not perfect, but it’s the first time in 7 years I’ve felt like myself. Don’t let fear stop you from trying. You deserve stability.
Rob Webber
February 2, 2026 AT 21:34Stop romanticizing these drugs. Methadone turns people into zombies. Buprenorphine is a placebo for weak addicts who can’t handle real withdrawal. If you can’t quit cold turkey, you weren’t serious to begin with. These meds are just corporate profit machines disguised as compassion. People don’t need medication-they need discipline. And maybe a good kick in the ass.
Lisa McCluskey
February 2, 2026 AT 23:55Constipation on methadone is brutal. I went from drinking 3L of water a day to using Miralax daily. It’s not just about pills-diet and movement matter. I started walking 45 minutes every morning. It helped more than I expected. And if you’re having sexual side effects, talk to your doctor. There are options. You’re not broken. Just adjusting.
April Allen
February 4, 2026 AT 08:49The pharmacodynamic ceiling effect of buprenorphine represents a fundamental divergence from full mu-opioid receptor agonism, which inherently limits its efficacy in high-tolerance populations. This ceiling, while conferring a superior safety profile regarding respiratory depression, may inadvertently reinforce non-adherence due to suboptimal symptom suppression. The resultant paradox-enhanced safety at the cost of therapeutic adequacy-demands a personalized, biopsychosocial framework for treatment selection rather than a one-size-fits-all paradigm. The data suggests that structural access disparities, not pharmacological inferiority, are the primary driver of attrition in buprenorphine cohorts.
Diana Dougan
February 5, 2026 AT 15:06Wow, so methadone makes you sleepy and buprenorphine tastes like plastic. Groundbreaking. I bet if you just stopped being lazy and did yoga instead, you wouldn’t need any of this. Also, why are we even talking about this? Isn’t addiction just a choice? I mean, I’ve never needed a pill to get through my day. Maybe you just need to try harder.
Bobbi Van Riet
February 6, 2026 AT 16:20I remember when I first started methadone-I was terrified of the heart risks. I asked for an EKG and they said no unless I was over 100mg. I was at 80, but I was scared. So I went to a private clinic and paid out of pocket. Best decision I ever made. Turned out my QT was borderline. They lowered my dose and now I’m fine. Don’t assume your doctor knows everything. Ask for tests. Push back. Your life matters more than their time.
Natasha Plebani
February 6, 2026 AT 18:44The ontological tension between pharmacological stabilization and existential autonomy is rarely addressed. We medicate to restore function, yet the very act of dependency on a regulated substance reconfigures identity. Is the person on methadone ‘sober’? Or are they merely chemically reoriented? The language of recovery must evolve beyond abstinence to encompass embodied continuity. We don’t need to eliminate dependence-we need to reframe it as a form of self-preservation, not surrender.
Eliana Botelho
February 8, 2026 AT 06:52Why are we even letting doctors prescribe this stuff? Why not just lock everyone up and force them to detox? It’s cheaper than all these meds and clinics. And why does buprenorphine need to be a film? Why not just make it a pill like normal medicine? This whole thing feels like a scam to make pharma rich while keeping addicts on a leash. Also, why do they say ‘don’t drink alcohol’ like that’s news? Of course you shouldn’t mix drugs and booze. Duh.
Darren Gormley
February 9, 2026 AT 18:50People don’t realize methadone is literally designed to keep you addicted. It’s not a cure-it’s a life sentence with a prescription. And buprenorphine? It’s the ‘lite’ version of the same prison. 🤡 The real solution? Abstinence. Hardcore. No meds. No excuses. But hey, if you want to live on government handouts and call it ‘recovery,’ go ahead. I’ll be over here living my life without needing a chemical crutch.
Mike Rose
February 10, 2026 AT 21:05Why do these articles always sound like they’re written by a pharma rep? Methadone = bad. Buprenorphine = good. But both are just drugs. People need to quit cold turkey. That’s it. No excuses. I did it. You can too. Stop reading this junk and go to a meeting. Or better yet, go to the gym. Sweat it out. Real recovery doesn’t come in a pill or a film.
Russ Kelemen
February 12, 2026 AT 17:35Hey, if you’re reading this and you’re on one of these meds-congrats. You’re still here. That’s more than most. Side effects suck, but they’re not the whole story. You’re not weak for needing help. You’re brave for staying. Talk to your provider. Adjust. Try new things. You’re not alone. I’ve been where you are. It gets better. Not perfect. But better. Keep going.
Adarsh Uttral
February 14, 2026 AT 17:32My cousin on methadone lost his job because he was too sleepy. But he got his license back after 6 months. Now he drives a truck. He says the constipation still sucks, but he’d rather be alive than high. I think these meds are messy but real. Not magic, not evil. Just tools. Use them right.