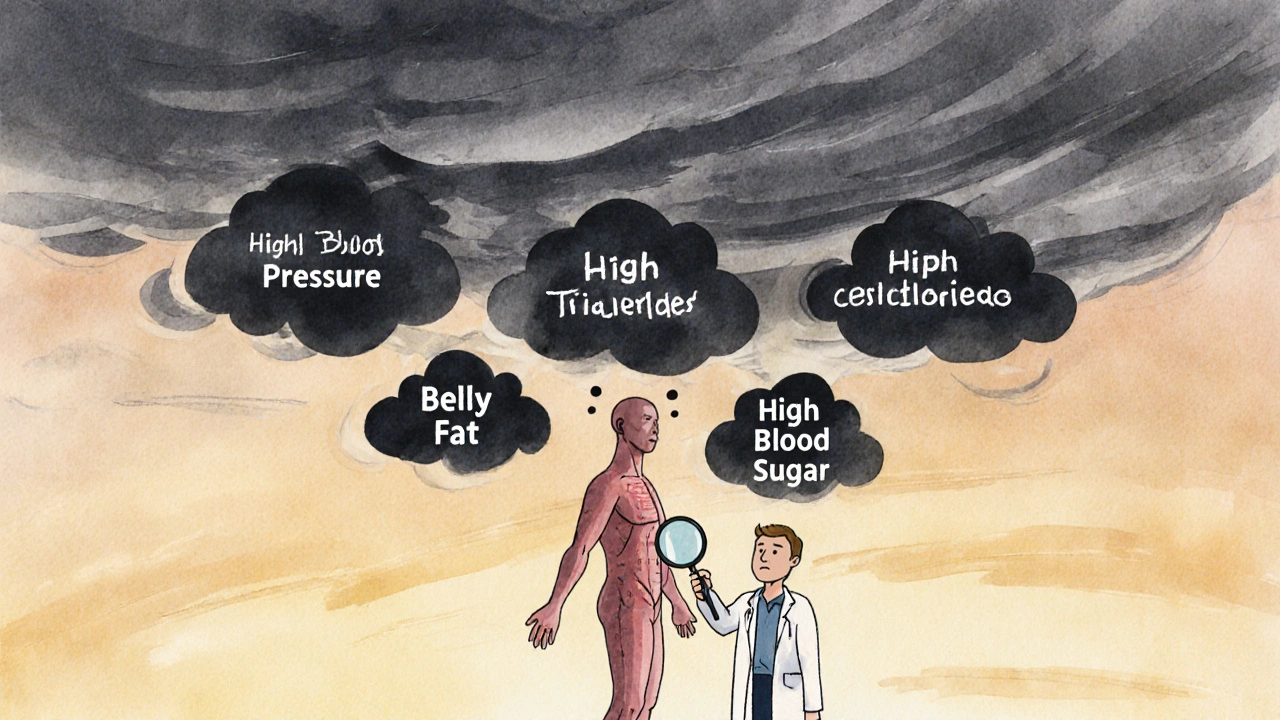
Imagine your body sending out warning signs - high blood pressure, a growing waistline, rising blood sugar, and strange cholesterol numbers - but your doctor only treats one of them. That’s the problem with metabolic syndrome. It’s not just one thing wrong. It’s five things happening together, quietly raising your risk of a heart attack, stroke, or type 2 diabetes long before you feel sick. And most people don’t even know they have it.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t a single disease. It’s a group of conditions that happen at the same time and make your heart and blood vessels work harder than they should. Think of it like a storm cloud gathering: high blood pressure, too much belly fat, high triglycerides, low good cholesterol, and elevated blood sugar. You don’t need all five to be in danger - just three of them.
The official criteria, set by the American Heart Association and the National Heart, Lung, and Blood Institute, are clear:
- Waist size over 40 inches for men, or 35 inches for women (lower for Asian populations)
- Triglycerides at or above 150 mg/dL
- HDL cholesterol below 40 mg/dL for men, or 50 mg/dL for women
- Blood pressure at or above 130/85 mmHg
- Fasting blood sugar of 100 mg/dL or higher
If you meet three or more, you have metabolic syndrome. And according to data from the National Health and Nutrition Examination Survey, nearly 35% of U.S. adults have it - that’s over 86 million people. The numbers climb with age: almost half of people over 60 are affected.
Why It’s More Dangerous Than Single Risk Factors
Having high blood pressure alone is bad. High cholesterol? Also bad. But when they show up together with belly fat and insulin resistance, they don’t just add up - they multiply. This is the real danger of metabolic syndrome.
The core driver? Insulin resistance. Your body’s cells stop responding properly to insulin, the hormone that moves sugar from your blood into your muscles and fat for energy. So your pancreas pumps out more insulin to compensate. That extra insulin doesn’t just raise blood sugar - it triggers inflammation, increases fat storage around your organs, and makes your blood pressure climb. It’s a domino effect.
Studies like the Framingham Heart Study show that people with metabolic syndrome have 1.5 to 2 times the risk of heart disease and five times the risk of developing type 2 diabetes compared to those without it. That’s not a small increase. That’s a red flag.
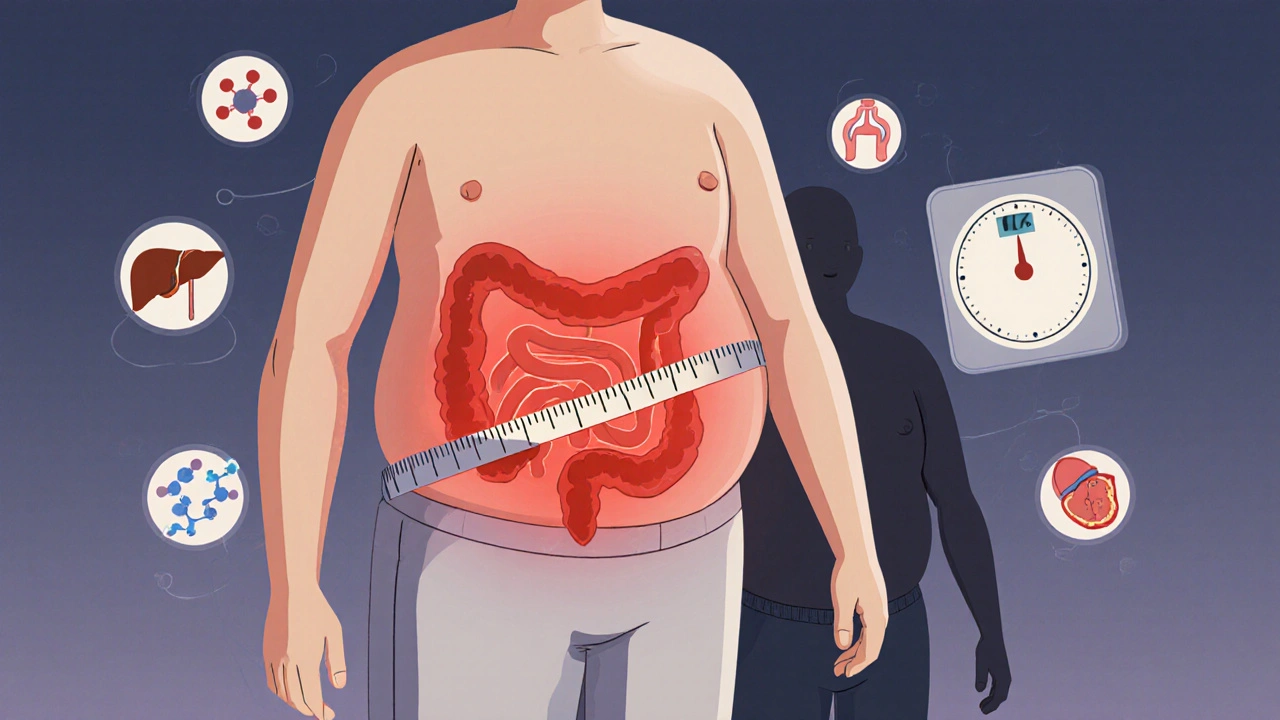
The Belly Fat Connection
Not all fat is the same. Subcutaneous fat - the kind you can pinch on your thighs or arms - isn’t the main culprit. It’s visceral fat. That’s the deep fat wrapped around your liver, pancreas, and intestines. It’s invisible, but it’s active. It releases fatty acids and inflammatory chemicals directly into your bloodstream, messing with your metabolism.
That’s why waist size matters more than total weight. Two people might weigh the same, but if one has a waist over 40 inches, they’re at much higher risk. Even people who aren’t overweight can have metabolic syndrome if they carry fat around their middle. This is why doctors now measure waistlines - not just BMI.
Who’s Most at Risk?
Metabolic syndrome doesn’t pick favorites, but it does have patterns. Age is a big one - risk jumps sharply after 40. But it’s also tied to lifestyle. Sedentary habits, diets heavy in processed carbs and sugar, and chronic stress all feed the fire.
There are also ethnic differences. Hispanic adults have the highest rates in the U.S. at 38.6%, followed by non-Hispanic whites at 34.2%, and non-Hispanic Blacks at 31.8%. Asian Americans develop the condition at lower waist measurements - which is why their cutoff is 35 inches for men and 31 inches for women.
Women with polycystic ovary syndrome (PCOS) are especially vulnerable. Hormonal imbalances in PCOS make insulin resistance worse, and many women with PCOS meet the full criteria for metabolic syndrome without realizing it.
Why Doctors Miss It
Here’s the frustrating part: many people with metabolic syndrome are told they’re “fine” because each individual number is only slightly out of range. High blood pressure? We’ll give you a pill. High cholesterol? Here’s a statin. Blood sugar’s a little up? Just watch your sugar intake.
But treating each piece separately misses the bigger picture. A 2022 survey on HealthUnlocked found that 68% of people with metabolic syndrome weren’t diagnosed - their doctors treated symptoms, not the syndrome. Reddit users in r/MetabolicSyndrome report feeling dismissed until they pushed for a full metabolic panel. Fragmented care is the norm. Cardiologists, endocrinologists, and primary care docs often work in silos, never seeing the full pattern.
How to Reverse It - Without Pills
There’s no magic drug for metabolic syndrome. No pill that fixes all five problems at once. But there is something better: lifestyle change. And it works - fast.
The Diabetes Prevention Program (DPP), one of the most studied interventions in medical history, showed that losing just 7% of your body weight and doing 150 minutes of walking per week cut the risk of developing type 2 diabetes by 58%. That same program also reduced metabolic syndrome by 41% over 10 years.
Here’s what actually moves the needle:
- Drop the sugar and refined carbs. White bread, pasta, soda, and pastries spike blood sugar and insulin. Swap them for whole grains, vegetables, legumes, and lean proteins.
- Move daily. You don’t need to run a marathon. Brisk walking, cycling, or swimming for 30 minutes, five days a week, improves insulin sensitivity within weeks.
- Target belly fat. Strength training helps build muscle, which burns more calories at rest. Combine it with cardio for best results.
- Sleep and manage stress. Poor sleep and high cortisol levels worsen insulin resistance. Aim for 7-8 hours a night and find ways to unwind - meditation, deep breathing, or even a daily walk.
One patient in the Mayo Clinic’s Integrated Metabolic Syndrome Program lost 22 pounds in six months, dropped his waist from 44 to 36 inches, and reversed all five risk factors - without medication.
What About Medications?
Medications can help manage individual pieces - statins for cholesterol, ACE inhibitors for blood pressure, metformin for blood sugar. But none of them target the syndrome as a whole. The American College of Cardiology now recommends that people with metabolic syndrome start statins earlier than usual because their overall risk is so high.
There’s also new tech. In January 2023, the FDA approved the first digital therapeutic for metabolic syndrome: DarioHealth’s Metabolic+ app. It uses continuous glucose monitoring and behavioral coaching to help users track their food, activity, and stress. In a trial, users lost 3.2 cm off their waist and lowered HbA1c by 0.6% in six months - results that rival traditional lifestyle programs.

Can It Be Reversed?
Yes. And not just managed - reversed.
The DiRECT trial in the UK showed that 46% of people with type 2 diabetes and metabolic syndrome achieved remission after losing 15 kg or more through a structured low-calorie diet and long-term support. Their blood pressure normalized, triglycerides dropped, HDL rose, and fasting glucose returned to normal. The syndrome disappeared.
It’s not easy. It takes discipline. But it’s not impossible. And the longer you wait, the harder it gets. Insulin resistance becomes more entrenched. Fat cells become more inflamed. Blood vessels start to stiffen.
The Bigger Picture
Metabolic syndrome isn’t just a personal health issue - it’s a public health crisis. In the U.S. alone, it costs $219 billion a year in medical bills and another $143 billion in lost work time. And it’s getting worse. Since 2000, the prevalence has jumped 35%, driven by rising obesity and sedentary lifestyles.
But here’s the hopeful part: it’s one of the most preventable conditions we have. Unlike genetic diseases or autoimmune disorders, metabolic syndrome responds powerfully to changes in diet, movement, and sleep. It’s a reminder that your daily choices - what you eat, how you move, how you rest - have a direct, measurable impact on your heart’s future.
If you’ve been told your numbers are “a little off,” don’t wait. Get your waist measured. Ask for a full lipid panel. Check your fasting glucose. Don’t let one doctor treat one number. Ask: “Could this be metabolic syndrome?”
Because the sooner you act, the more of your life you get to keep - and the less likely you are to end up in a hospital because your heart gave out.
Can you have metabolic syndrome without being overweight?
Yes. While obesity - especially abdominal fat - is the most common cause, some people with normal weight can still have metabolic syndrome. This is called "TOFI" - thin outside, fat inside. Visceral fat can accumulate even if your overall weight is normal, especially if you’re inactive or eat a lot of processed carbs. Waist measurement is more important than BMI.
Is metabolic syndrome the same as prediabetes?
No, but they often overlap. Prediabetes means your blood sugar is higher than normal but not yet diabetic. Metabolic syndrome includes prediabetes as one of five possible components. You can have prediabetes without the other four factors - and you can have metabolic syndrome without prediabetes if your fasting glucose is borderline. But if you have both, your risk of heart disease and diabetes skyrockets.
How long does it take to reverse metabolic syndrome?
Significant improvements can happen in as little as 6 months. Losing 5-7% of your body weight, getting 150 minutes of exercise weekly, and cutting out sugary drinks and refined carbs can normalize blood pressure, triglycerides, and fasting glucose. Many people see two or more risk factors disappear within this timeframe. Full reversal - meeting none of the five criteria - often takes 12-18 months of consistent effort.
Does alcohol affect metabolic syndrome?
Yes - but it’s complicated. Heavy drinking raises triglycerides and blood pressure and worsens insulin resistance. However, moderate alcohol intake (one drink per day for women, two for men) may slightly raise HDL cholesterol. The key is moderation. If you have metabolic syndrome, it’s safer to limit or avoid alcohol, especially if your triglycerides are already high.
Can children get metabolic syndrome?
Yes - and it’s rising fast. With childhood obesity rates climbing, more kids are developing the same risk factors as adults. The American Academy of Pediatrics now recommends screening overweight children (BMI over 85th percentile) for high blood pressure, cholesterol, and blood sugar starting at age 10. Early intervention with diet and activity can prevent lifelong complications.
What to Do Next
If you’re worried you might have metabolic syndrome, start here:
- Measure your waist - right now. If it’s over 40 inches (men) or 35 inches (women), that’s a red flag.
- Ask your doctor for a fasting blood test: glucose, triglycerides, HDL, and a full lipid panel.
- Get your blood pressure checked multiple times over a week - one reading isn’t enough.
- Start walking 30 minutes a day, five days a week. No gym needed.
- Remove sugary drinks, white bread, and pastries from your home. Replace them with water, vegetables, beans, and whole grains.
You don’t need a miracle. You need consistency. And the best part? Every small change you make today reduces your risk - not just for heart disease, but for stroke, kidney failure, and dementia too. Metabolic syndrome isn’t a life sentence. It’s a call to action - and you’re the only one who can answer it.

Esperanza Decor
November 12, 2025 AT 03:48This article hit me right in the gut. I didn’t realize my waistline was the real red flag-not my weight. I’ve been told I’m ‘just a little chubby’ for years, but when I measured myself last week, I was at 41 inches. No wonder my triglycerides are through the roof. I started walking after dinner every night and cut out soda. Two weeks in, my blood pressure dropped 10 points. It’s not magic, but it’s real.
Deepa Lakshminarasimhan
November 12, 2025 AT 04:46They say it’s lifestyle but what if it’s the food additives? Glyphosate in corn syrup, endocrine disruptors in plastic packaging, the government’s been pushing processed carbs for decades so Big Pharma can sell more statins. No one talks about the real poison. They just want you to walk more and blame yourself.
Erica Cruz
November 13, 2025 AT 13:25Let’s be real-this whole ‘metabolic syndrome’ thing is just a fancy way for doctors to sell more tests and meds. If you’re not obese, why are you being pathologized? My cousin has a 38-inch waist and runs marathons. His bloodwork is perfect. This isn’t science-it’s fearmongering dressed up as prevention.
Johnson Abraham
November 14, 2025 AT 13:30lol i thought this was gonna be about how sugar kills u but now i see its just another ‘walk more’ post. bro i got a 42 inch waist and i work 60 hrs a week. what am i sposed to do, nap between meetings? also my doc gave me a statin and said ‘good luck’.
Shante Ajadeen
November 15, 2025 AT 09:04I was skeptical at first, but I did the 30-minute walk thing every day for a month and swapped out my afternoon cookie for almonds. My fasting glucose dropped from 108 to 92. I didn’t even realize how tired I was until I started feeling energy again. You don’t need to overhaul your life-just start small. And you’re not alone in this.
dace yates
November 17, 2025 AT 08:12Does anyone know if intermittent fasting helps with visceral fat specifically? Or is it just overall calorie reduction that matters? I’ve read conflicting things and I’m trying to figure out if timing matters as much as what I eat.
Danae Miley
November 19, 2025 AT 06:17Correction: The DiRECT trial showed 46% remission in type 2 diabetes patients with metabolic syndrome after 15kg weight loss-but remission was defined as HbA1c <6.5% without medication for at least 6 months. The original paper (Lancet 2018) is clear: it’s not ‘reversal’ unless all five criteria are met. Don’t oversimplify the science.
Charles Lewis
November 19, 2025 AT 22:12It’s important to recognize that metabolic syndrome is not merely a collection of biomarkers-it is a systemic dysregulation of energy homeostasis, driven by chronic low-grade inflammation and insulin resistance, often exacerbated by environmental and socioeconomic determinants of health. The individualistic framing of ‘just walk more’ ignores the structural realities faced by many: food deserts, lack of safe recreational spaces, and the psychological toll of chronic stress. True intervention requires policy-level change alongside personal action. We must advocate for community gardens, subsidized healthy food, and workplace wellness programs-not just tell people to buy kale.