Medication Nausea Risk Calculator
Prevent Medication-Induced Nausea
This tool estimates your risk of nausea from medications and provides personalized prevention strategies based on your inputs.
Almost everyone has felt it - that sudden wave of queasiness after popping a pill, followed by the urge to throw up. It’s not just unpleasant; it can make you skip doses, delay treatment, or even stop taking life-saving medications. Nausea and vomiting from medications are among the most common side effects, affecting millions every year. The good news? You don’t have to just endure it. There are real, proven ways to prevent it and find relief - without waiting for symptoms to get worse.
Why Some Medications Make You Sick
Not all nausea is the same. When a drug causes vomiting or queasiness, it’s usually hitting one of three targets in your body: your stomach lining, the chemoreceptor trigger zone in your brain, or the vomiting center in your brainstem. Some medications, like antibiotics or NSAIDs, directly irritate your stomach. Others, like chemotherapy drugs or opioids, activate nerve pathways that tell your brain it’s being poisoned - even if it’s not. The worst offenders? Chemotherapy drugs top the list. Without prevention, up to 80% of patients on strong chemo get sick. But even common pills like ibuprofen, multivitamins, and SSRIs can trigger nausea. The timing matters too. Symptoms often hit hardest in the first few days after starting a new drug, when your body is still adjusting.Start with What’s in Your Kitchen
Before reaching for another pill, try the simplest, cheapest, and safest fixes first. Many people don’t realize that how and when they take their meds makes a huge difference. Take your medicine with food - unless your doctor says not to. Antibiotics, NSAIDs, and iron supplements are notorious for stomach upset. Eating even a small snack like toast, crackers, or yogurt can shield your stomach lining. Don’t wait until you feel sick to eat. Keep light snacks handy, especially if you’re on a new drug. Ginger is one of the most backed natural remedies. Studies and patient reports show ginger chews, tea, or capsules can cut nausea by half. One cancer patient on Reddit said ginger chews every two hours dropped their nausea from an 8 out of 10 to a 3 in less than a day. Keep a pack of ginger chews in your bag, or sip ginger tea before taking pills. Stay hydrated, but sip slowly. Dehydration makes nausea worse. Water, clear broths, or electrolyte drinks help. Avoid sugary sodas or heavy juices - they can make stomach upset worse. Sipping cold fluids through a straw can feel easier on your system. Avoid spicy, greasy, or overly sweet foods. These are harder to digest and can amplify nausea. Stick to bland, carb-heavy options: rice, plain pasta, bananas, applesauce. The American Cancer Society says avoiding your favorite foods during treatment helps you keep enjoying them later - no bad associations.Environment and Mindset Matter
Your surroundings can make nausea better or worse. If you feel queasy, get fresh air. Open a window, step outside for a few minutes, or sit near a fan. Cool air helps reset your senses. Relaxation techniques aren’t just for stress. Deep breathing, meditation, and progressive muscle relaxation have been shown to reduce nausea in clinical settings. Try inhaling slowly through your nose for four counts, holding for four, then exhaling through your mouth for six. Repeat five times. Do this before taking pills, or when you feel the first wave of nausea. Avoid strong smells. Cooking odors, perfume, cigarette smoke, and even cleaning products can trigger vomiting. If you’re sensitive, ask someone else to cook, or use unscented products.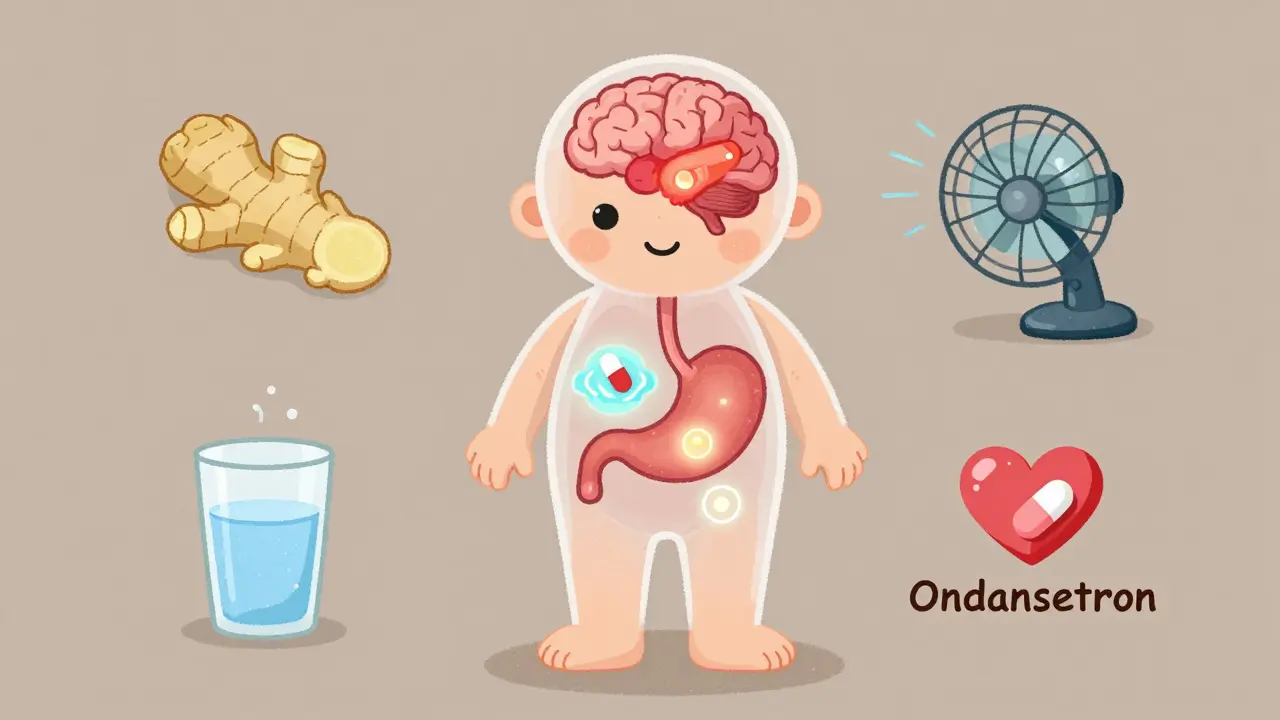
When Pills Are Needed - The Right Ones for the Right Situation
If lifestyle changes aren’t enough, there are effective medications designed to block nausea at its source. But not all antiemetics work the same way - and not all are right for every drug. For chemotherapy, the gold standard is a three-drug combo: a 5-HT3 blocker like ondansetron (Zofran), an NK-1 blocker like aprepitant (Emend), and dexamethasone. This combo works in 75-85% of cases for acute nausea and still controls 65-75% of delayed nausea. For moderate chemo, two drugs - ondansetron plus dexamethasone - are usually enough. For post-surgery nausea, a mix of ondansetron and dexamethasone given before discharge cuts post-op vomiting by nearly 20% compared to ondansetron alone. Some hospitals now use a simple rule: if you’re a woman who doesn’t smoke, you get three drugs. Men get two. This cuts nausea rates from 46% down to 18%. For everyday nausea from antibiotics or painkillers, ondansetron or metoclopramide (Reglan) may be prescribed. But metoclopramide has risks - long-term use can cause involuntary movements - so it’s not first-line unless other options fail. Mirtazapine, an antidepressant, is sometimes used off-label for nausea. At low doses (15-30 mg), it blocks serotonin receptors and can reduce post-op nausea by 40-60%. It’s also sedating, so it’s often taken at night - which helps if your nausea is worse when lying down. Tricyclic antidepressants like nortriptyline can help chronic functional nausea, but they don’t work for everyone. A 2021 study found they helped 51% of patients with long-term nausea - but another trial showed no benefit for gastroparesis. That’s why doctors test them case by case.What Not to Do
Many people try to tough it out - and pay the price. Skipping doses because you’re nauseated can make your original condition worse. One survey found 35% of patients reduced or stopped their meds without telling their doctor because they couldn’t afford antiemetics or thought the nausea was normal. Don’t assume all nausea is from your pill. Sometimes it’s something else: a stomach bug, anxiety, dehydration, or even another medication interacting. If nausea starts weeks after beginning a drug, or if it’s accompanied by dizziness, fever, or abdominal pain, talk to your provider. Don’t just blame the medicine. Avoid alcohol with nausea-triggering drugs. It increases stomach irritation and can worsen vomiting. Same with caffeine - it can stimulate the nervous system and make nausea more intense. Don’t rely on over-the-counter motion sickness patches or Dramamine unless advised. They work for inner-ear dizziness, not drug-induced nausea, and can cause drowsiness that interferes with daily life.Cost and Access - A Real Barrier
The most effective antiemetics aren’t cheap. A single dose of aprepitant can cost $150-$300 without insurance. Many patients skip them because of price - even when their doctor recommends them. Ask about generics. Ondansetron is available as a cheap generic. Dexamethasone is inexpensive too. Some pharmacies offer discount programs for NK-1 blockers. Your oncologist or pharmacist might know about patient assistance programs from drug manufacturers. If cost stops you from taking your meds, tell your provider. There are alternatives. Sometimes switching to a different antibiotic or painkiller can cut nausea without losing effectiveness.
When to Call Your Doctor
Not every case of nausea needs a prescription. But if any of these happen, reach out:- You’ve vomited more than twice in 24 hours
- You can’t keep down fluids for more than 12 hours
- You feel dizzy, confused, or your heart races
- Nausea lasts longer than a week after starting the drug
- You’re losing weight or feel unusually weak
What’s New in 2026
The field is evolving. In 2023, the FDA approved rolapitant (Varubi) for children as young as 2 with chemotherapy-induced nausea - a big step forward. Hospitals are now piloting apps like Nausea Tracker, where patients log symptoms daily. These help doctors spot patterns and adjust meds faster. Behavioral therapy is gaining traction too. For anticipatory nausea - that dread-induced queasiness before chemo - cognitive behavioral therapy (CBT) is now recommended by the American Psychosocial Oncology Society. It helps retrain your brain to stop linking treatment with sickness. Some clinics are testing genetic tests to predict who responds best to which antiemetic. This could mean fewer trial-and-error prescriptions in the future.Final Thoughts: You’re Not Alone, and It Doesn’t Have to Be This Way
Nausea from medication isn’t a sign you’re weak or doing something wrong. It’s a biological reaction - and one that can be managed. Start with food, ginger, and fresh air. If that’s not enough, ask about antiemetics. Don’t let cost or fear stop you from speaking up. Your doctor’s job isn’t just to treat your illness - it’s to help you live through treatment with as little suffering as possible.Most people who try a combination of these strategies find relief. You can too.
Can I take ginger with my prescription meds?
Yes, ginger is generally safe with most medications, including antibiotics and chemotherapy drugs. But if you’re on blood thinners like warfarin, talk to your doctor first - ginger can have mild blood-thinning effects. For most people, ginger chews, tea, or capsules (250-500 mg) taken 3-4 times a day are well tolerated and effective.
Why does nausea get worse at night?
Lying down slows digestion and can cause stomach acid to rise, making nausea feel stronger. Some medications also peak in your bloodstream at night. Taking your pill earlier in the day, or using a bedtime antiemetic like mirtazapine, can help. Also, avoid eating heavy meals within two hours of bedtime.
Do anti-nausea pills cause drowsiness?
Some do, some don’t. Ondansetron usually doesn’t cause sleepiness. Dexamethasone might keep you awake. Mirtazapine and older drugs like promethazine can make you very drowsy. If you need to stay alert, ask your doctor for non-sedating options. Timing matters too - taking sedating meds at night can turn a side effect into a benefit.
How long does medication-induced nausea last?
It depends on the drug. For antibiotics or NSAIDs, nausea usually fades within 3-7 days as your body adjusts. Chemo-induced nausea can last longer - up to 5-7 days after treatment, especially delayed nausea. If it lasts more than a week without improvement, it’s not normal. Talk to your provider. There might be a better drug option or an added antiemetic.
Can I prevent nausea before starting a new medication?
Absolutely. Ask your doctor or pharmacist: "Is nausea common with this drug? What’s the best way to prevent it?" Many providers now give antiemetics upfront - especially for chemo, opioids, or certain antibiotics. Start with food, ginger, and hydration before the first dose. Don’t wait until you’re sick to act.
If you’re on a new medication and feel queasy, you’re not broken. You’re human. And with the right tools, you can keep taking what you need - without the sickness.


Adam Rivera
January 13, 2026 AT 16:41Just took my antibiotics with a spoonful of peanut butter and some ginger tea-no nausea at all. Seriously, why didn’t anyone tell me this sooner? Food isn’t the enemy, it’s your first line of defense.
Rosalee Vanness
January 14, 2026 AT 17:18I’ve been on SSRIs for three years and still get that wave of nausea every time I switch brands. What saved me? Cold ginger ale sipped through a straw while sitting in front of a fan. It’s not glamorous, but it’s real. And honestly? The fact that you mentioned avoiding favorite foods during treatment-that hit me in the chest. I stopped eating sushi for six months because I associated it with puking. Now I can enjoy it again. Small wins, y’all.
lucy cooke
January 15, 2026 AT 06:11Oh, how quaint. You suggest ginger? As if the ancient wisdom of rhizomes can outmaneuver the sophisticated pharmacodynamics of modern neuropharmacology? One must ask: is this not merely a capitulation to folk medicine in an age of evidence-based science? And yet… I tried it. After my third cycle of cisplatin, when ondansetron failed, I chewed ginger like a monk chewing mantras-and the queasiness receded like a tide of existential dread. I am now a reluctant convert. The universe, it seems, still whispers through roots.
Trevor Davis
January 17, 2026 AT 05:52Guys. I’m not even kidding. I took Zofran, then drank a protein shake, then threw up both. Then I ate a single saltine cracker and took my pill with water. No vomit. No nothing. Sometimes the answer isn’t more drugs-it’s less chaos. Also, don’t lie down right after. I learned that the hard way. Like, sobbing-on-the-bathroom-floor hard.
John Tran
January 18, 2026 AT 15:55So i read this whole thing and like… why is everyone so obsessed with ginger? Like its some magic herb? I mean sure its kinda helpful but its not like its a cure-all. And also i think the part about mirtazapine is kinda sketchy because i tried it for anxiety and it made me feel like a zombie who forgot how to walk. Also i think the cost thing is bs-my cousin got all her chemo meds covered by medicaid and still complained. People just dont wanna try harder. Also i think the FDA should just ban all nausea causing drugs. Simple.
Trevor Whipple
January 18, 2026 AT 17:38Ugh. Of course you’re gonna get sick if you’re taking random pills. If you can’t handle your meds, maybe you shouldn’t be on them. I’ve been on 12 different antibiotics and never thrown up once. Why? Because I take them with food, not while scrolling TikTok. Also, ginger? That’s for people who don’t know what a proton pump inhibitor is. Get real.
Lethabo Phalafala
January 19, 2026 AT 17:07I’m from Johannesburg and we don’t have access to half these drugs. But we have rooibos tea, lemon, honey, and silence. My aunt survived chemo with nothing but those three things and a prayer. I didn’t believe it until I saw her. No fancy pills. Just presence. Maybe the real medicine isn’t in the bottle-it’s in the way we hold space for each other when the world feels like it’s spinning.
Nelly Oruko
January 20, 2026 AT 01:08Did anyone else notice the typo in the section on NK-1 blockers? It says 'aprepitant (Emend)' but the brand is Emend®. Small detail, but precision matters when discussing pharmacology. Also-ginger works. I’ve used it for morning sickness and chemo. 500mg capsules, 4x/day. No drowsiness. No drama. Just relief.
vishnu priyanka
January 20, 2026 AT 12:56From India, where ginger is in everything-chai, curry, even toothpaste. We’ve known this for centuries. But here’s the twist: we also use ajwain seeds (carom) crushed in warm water. It’s like ginger’s quieter, spicier cousin. Works like a charm for antibiotic nausea. And yes, we take it with roti, not on an empty stomach. Tradition isn’t magic-it’s accumulated wisdom. Also, no one talks about how sleep position affects nausea. Side-sleeping > back. Try it.
Diana Campos Ortiz
January 20, 2026 AT 22:19Thank you for writing this. I’ve been too ashamed to tell my doctor I skipped my antidepressant for two weeks because I couldn’t stomach it. I thought I was weak. Turns out, I just needed ginger and a cracker. I’m starting again tomorrow. And I’m telling my doctor about the cost issue. I’m not broken. I’m just human.
Jesse Ibarra
January 22, 2026 AT 04:51Wow. So much ‘compassion’ and ‘you’re not alone’ nonsense. Let’s be real: if you can’t tolerate your meds, you’re not a victim-you’re a liability. Your body’s rejecting treatment. Maybe the real problem isn’t the nausea-it’s that you shouldn’t be on that drug in the first place. Stop treating nausea like a spiritual journey. Get a better prescription. Or stop being a drama queen.
laura Drever
January 22, 2026 AT 10:38lol ginger. also why is everyone acting like this is new info. i learned this from my grandma in 1997. also the part about avoiding favorite foods? that’s not science thats just sad. and why is this 10 pages long? just tell people take it with food and dont drink alcohol. done. over.
James Castner
January 23, 2026 AT 07:46As a clinical pharmacologist with over two decades of experience in oncology and neuropharmacology, I must commend the depth of this exposition-particularly the nuanced differentiation between acute and delayed chemotherapy-induced nausea and vomiting (CINV), and the precise delineation of receptor-specific antiemetic mechanisms. However, I must also register a formal objection to the uncritical elevation of ginger as a primary intervention. While ginger’s 5-HT3 receptor antagonism is documented in randomized controlled trials (e.g., *Journal of Clinical Oncology*, 2012), its bioavailability is highly variable, and its pharmacokinetic profile lacks the predictability required in clinical settings where therapeutic precision is non-negotiable. To suggest that a dietary supplement can supplant the gold-standard triple regimen of NK-1/5-HT3/dexamethasone is not merely reductionist-it is potentially dangerous. That said, the integration of behavioral interventions, such as CBT for anticipatory nausea, represents a paradigm shift worthy of institutional adoption. I would further propose that future iterations of this guide include pharmacogenomic screening for CYP2D6 and CYP3A4 polymorphisms, which significantly influence ondansetron metabolism and efficacy. To the patient who asked about cost: you are not alone. But neither are you powerless. Advocate. Document. Demand. The system is broken, but your voice is the scalpel that can cut through it.