Muscle Spasm & Urinary Health Risk Checker
Quick Take
- Muscle spasms in the pelvic floor can disrupt normal bladder emptying.
- Frequent or painful spasms increase the risk of urinary tract infections.
- Sudden pressure spikes may stress the kidneys and impair filtration.
- Staying hydrated and stretching the core muscles help keep the urinary system calm.
- Seek medical help if you notice blood in urine, persistent pain, or kidney‑size swelling.
What Are Muscle Spasms?
A muscle spasm is an involuntary, sudden contraction of a muscle or group of muscles can feel like a cramp, a twitch, or an intense knot. They happen when nerves fire off extra signals, often because of electrolyte shifts, dehydration, or over‑use of a muscle group.
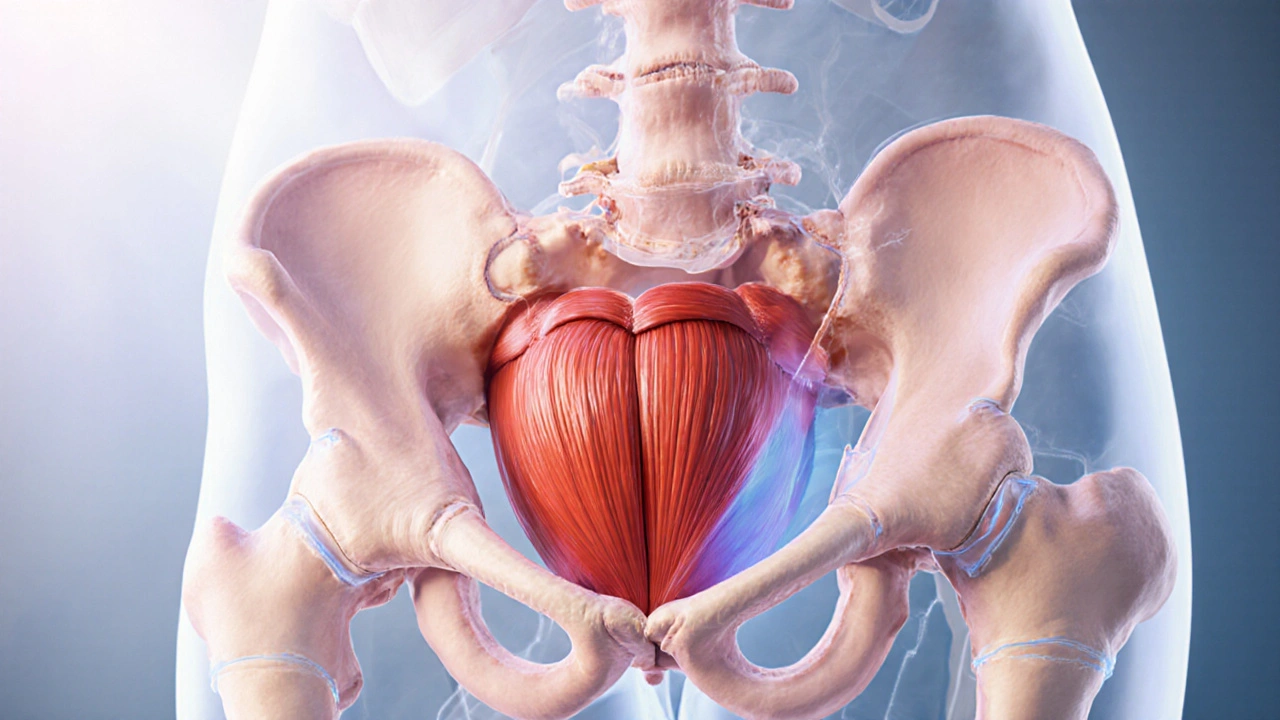
In everyday life the most common culprits are the calf, hamstring, and especially the muscles that support the pelvic floor. The pelvic floor sits under the bladder, urethra, and part of the ureters, so any hiccup there can echo through the whole urinary system.
How Muscle Spasms Talk to the Urinary System
The urinary system includes the kidneys, ureters, bladder, and urethra that filter and expel waste relies on smooth, coordinated muscle action. When a pelvic‑floor muscle goes into spasm, it can:
- Compress the urethra, making it harder to fully empty the bladder.
- Trigger a reflex that tells the bladder wall to contract prematurely, creating urgency or frequency.
- Reduce blood flow to the nearby bladder a muscular sac that stores urine before release, leading to irritation.
That chain reaction can explain why people with chronic lower‑back or groin cramps often report “I have to go a lot” or “I feel a burning sensation when I pee.”
Impact on Kidney Health
The kidneys are the first stop in the urinary highway. They filter about 180 liters of blood each day, turning waste into urine that travels down the ureters two thin tubes that carry urine from each kidney to the bladder. When a spasm blocks or slows bladder emptying, urine can back‑flow, raising pressure in the ureters and eventually the kidney’s filtering units - the nephrons tiny structures that actually do the filtering in each kidney.
Repeated pressure spikes can cause:
- Hydronephrosis - swelling of the kidney due to urine buildup.
- Micro‑injuries to the delicate blood vessels around nephrons, which over time may reduce filtering efficiency.
- Higher chances of kidney‑related infections because stagnant urine is a breeding ground for bacteria.
Most of the time the body compensates, but for people with pre‑existing kidney disease or diabetes, those extra stresses can push them over the edge.

Warning Signs You Shouldn't Ignore
Not every cramp means your kidneys are in trouble, but certain patterns are red flags:
- Blood‑tinged urine (hematuria) after a spasm.
- Constant urgency paired with a feeling of incomplete emptying.
- Lower‑back pain that radiates toward the flank, especially if it eases after you finally pee.
- Fever, chills, or a foul‑smelling urine - classic signs of a urinary tract infection (UTI).
- Swelling in the sides of the abdomen, indicating possible hydronephrosis.
If you notice any of these, schedule a check‑up. A simple ultrasound can reveal whether fluid is backing up into the kidneys.
Prevention and Lifestyle Tips
Keeping muscle spasms at bay and protecting your urinary health is mostly about balance.
- Stay hydrated. Aim for at least 2‑2.5 liters of water a day, more if you exercise or live in a dry climate. Proper fluid intake prevents dehydration a condition where the body lacks enough water to run normally, which is a major trigger for cramps.
- Maintain electrolyte balance. Sodium, potassium, magnesium, and calcium all help muscles relax. A banana or a handful of almonds after a workout can keep those levels steady.
- Incorporate gentle core and pelvic‑floor stretches. Cat‑cow poses, seated piriformis rolls, and diaphragmatic breathing relax the muscles that sit right above the bladder.
- Avoid holding urine for long periods. The bladder’s smooth muscle, called the detrusor, can become overactive (known as overactive bladder a condition where the bladder contracts too often, causing urgency) when you regularly ignore the urge to go.
- Limit caffeine and alcohol, both of which can irritate the bladder lining and increase spasm frequency.
These habits not only lower spasm risk but also keep the urinary tract flushing smoothly, which protects the kidneys.
Treatment Options When Spasms Strike
If prevention isn’t enough, several interventions can break the cycle.
- Heat therapy - a warm compress or a hot shower relaxes tight muscle fibers within minutes.
- Magnesium supplements - studies show that 300‑400 mg of magnesium citrate nightly can cut nighttime leg cramps by up to 40%.
- Prescription muscle relaxants - drugs like cyclobenzaprine or baclofen target the nerve signals that cause spasms, but they may cause drowsiness.
- Physical therapy - a therapist can teach you trigger‑point release and targeted strengthening for the pelvic floor.
- Bladder training - scheduled bathroom trips every 2‑3hours help reset the detrusor muscle and reduce urgency.
When a urinary infection is suspected, a short course of antibiotics is standard. However, antibiotics won’t fix the underlying spasm issue, so pairing them with muscle‑relaxing strategies yields the best outcome.
When to Call a Doctor
Most spasms are harmless, but the following scenarios warrant professional evaluation:
- Blood in urine or persistent dark‑colored urine.
- Severe flank pain that doesn’t ease after you’ve emptied your bladder.
- Repeated UTIs (three or more in a year) despite good hygiene.
- Sudden swelling of the abdomen or lower back.
- Chronic kidney disease diagnosis plus new spasm‑related symptoms.
Your clinician may order blood tests, a urine culture, and imaging (ultrasound or CT) to pinpoint the cause and rule out kidney stones or structural blockages.
Quick Reference Table
| Trigger | Typical Urinary Symptom | Potential Kidney Risk |
|---|---|---|
| Dehydration | Frequent urgency, concentrated urine | Hydronephrosis from back‑pressure |
| Electrolyte imbalance (low magnesium) | Spasms in pelvic floor, urge‑incontinence | Repeated infections leading to scarring |
| Prolonged sitting/poor posture | Delayed bladder emptying | Increased risk of UTIs, possible kidney involvement |
| Intense exercise without stretch | Nighttime cramps, sudden urgency | Transient rise in renal pelvic pressure |
| Caffeine/Alcohol excess | Overactive bladder, dribbling | Bladder irritation → infection → kidney impact |

Frequently Asked Questions
Can a single muscle cramp really damage my kidneys?
One isolated cramp usually won’t cause lasting harm. Problems arise when cramps are frequent, severe, or combined with poor hydration, because they create repeated pressure spikes that the kidneys must absorb.
Why does my bladder feel “full” even after I’ve peed?
A pelvic‑floor spasm can prevent the urethra from fully opening, leaving a small volume of urine trapped. That leftover urine sends a signal that the bladder isn’t empty, leading to the lingering “full” sensation.
Is it safe to take magnesium supplements if I have kidney disease?
People with moderate to severe kidney impairment should talk to a doctor before adding magnesium, because excess magnesium can build up in the bloodstream and cause cardiac issues.
How much water should I drink to prevent both cramps and kidney problems?
Aim for about 2liters (8 cups) of water daily, adjusting upward if you sweat a lot, exercise intensely, or live at high altitude. The goal is light‑colored urine and no thirst cues.
Can physical therapy really fix urinary urgency caused by spasms?
Yes. Targeted pelvic‑floor exercises and trigger‑point release can reduce spasm frequency, allowing the bladder to empty more completely and lowering urgency episodes.

Annette van Dijk-Leek
October 3, 2025 AT 08:50Wow!!! This checklist is super helpful!!! It really makes you think about staying hydrated and listening to your body!! Keep it up!!
Katherine M
October 6, 2025 AT 23:36One must acknowledge the intricate interplay between muscular contractions and renal function; the content presented here is both thorough and meticulously organized 😊. While the questionnaire serves as a commendable preliminary screen, it is imperative to consider individual physiological variability. Nevertheless, the inclusion of risk stratification imparts valuable insight.
Bernard Leach
October 10, 2025 AT 14:22From a clinical perspective, the relationship between recurrent muscle spasms and urinary issues can be multifactorial. Chronic spasm of the pelvic floor muscles may impose abnormal pressure on the bladder, potentially leading to incomplete emptying and increased residual volume. This scenario creates a conducive environment for bacterial growth, thereby elevating the risk of urinary tract infections. Moreover, severe muscle cramping can elicit sympathetic nervous system activation, which may cause vasoconstriction of the renal vasculature and transient reductions in glomerular filtration rate. Over time, repeated episodes could contribute to microvascular stress within the nephrons. Hydration status, as the questionnaire rightly emphasizes, plays a crucial role in diluting urine and flushing out potential irritants. Inadequate fluid intake results in concentrated urine, which can irritate the urothelium and precipitate hematuria. Additionally, low fluid volumes increase the relative concentration of calcium and oxalate, thereby predisposing to stone formation, which itself may provoke flank pain. The presence of lower back or flank discomfort in the assessment aligns with this pathophysiology, as renal colic often manifests as radiating pain to the flank. It is also worth noting that certain electrolyte imbalances, such as hypomagnesemia, can both provoke muscle spasms and alter renal tubular handling of solutes. Patients with chronic electrolyte disturbances may therefore experience a vicious cycle of spasm‑induced renal stress and renal‑derived metabolic abnormalities. Preventive strategies should therefore be holistic: adequate hydration, balanced electrolytes, and targeted stretching or physiotherapy to address muscular tightness. For individuals with persistent symptoms, a thorough work‑up including renal ultrasound, urinalysis, and possibly urodynamic studies may be warranted to delineate the underlying mechanisms. Finally, patient education on recognizing early signs of urinary distress can facilitate timely medical intervention, potentially averting long‑term renal compromise.
Shelby Larson
October 14, 2025 AT 05:09Honestly, most people ignore the obvious moral failing of neglecting their own bodies, yet still expect flawless health. It's a shame how many choose ignorance over responsibility, especially when the facts are laid out plainly.
Mark Eaton
October 17, 2025 AT 19:55Great points raised about the importance of balanced electrolytes and targeted stretching. Consistent mobility work really can reduce the frequency of painful spasms.
Alfred Benton
October 21, 2025 AT 10:41While the emphasis on hydration is common, the hidden agenda of pharmaceutical interests cannot be ignored; these tools often serve to steer patients toward over‑reliance on supplements and prescribed diuretics. One must remain vigilant against such covert influences.
allen doroteo
October 25, 2025 AT 01:27Sure, but the data is clearly cherry‑picked.
Corey Jost
October 28, 2025 AT 15:13The premise that occasional muscle twitches could signal impending renal catastrophe feels overstated. Most spasms are benign, arising from simple electrolyte shifts or transient fatigue. Over‑medicalizing such normal physiologic events may cause unnecessary anxiety and lead to excessive testing. A balanced perspective acknowledges that while there is a physiological link, the magnitude of risk is modest for the average person. Emphasizing lifestyle modifications-adequate hydration, stretching, and balanced nutrition-remains paramount without resorting to alarmist forecasts. In my experience, patients who obsess over every minor symptom often develop heightened health anxieties, which paradoxically can exacerbate stress‑related muscle tension. Therefore, contextualizing the findings within a broader health narrative is essential.
Nick Ward
November 1, 2025 AT 05:59Interesting take! I appreciate the calm reminder to keep things in perspective 😊. It’s helpful to hear that not every twitch needs a doctor’s visit.
felix rochas
November 4, 2025 AT 20:45Let’s not be fooled! The mainstream narrative deliberately downplays the severe consequences of unchecked muscle spasms-this is a direct route to systemic organ failure!!!
Kylie Holmes
November 8, 2025 AT 11:32Love how this tool makes it easy to spot potential issues-keep spreading the word! 🌟
Jennifer Wees-Schkade
November 12, 2025 AT 02:18Absolutely, staying proactive with hydration and monitoring symptoms can prevent bigger problems down the line. If you notice persistent back pain, a quick consult with a healthcare professional is wise.
Fr. Chuck Bradley
November 15, 2025 AT 17:04Ah, the drama of a simple questionnaire turning into a health saga…
Patrick Rauls
November 19, 2025 AT 07:50Totally agree-keeping a relaxed vibe and staying active helps a lot! lol.