When you're pregnant, taking folic acid isn't just a suggestion-it's a medical necessity. The neural tube, which becomes your baby’s brain and spine, closes by day 28 after conception. Most women don’t even know they’re pregnant by then. That’s why doctors tell you to start taking folic acid before you conceive. But here’s the part no one talks about enough: folic acid doesn’t play nice with every medication you might be on. And if you’re taking prenatal vitamins with iron, calcium, or anticonvulsants, you could be reducing its effectiveness-or even putting your baby at risk.
Why Folic Acid Matters More Than You Think
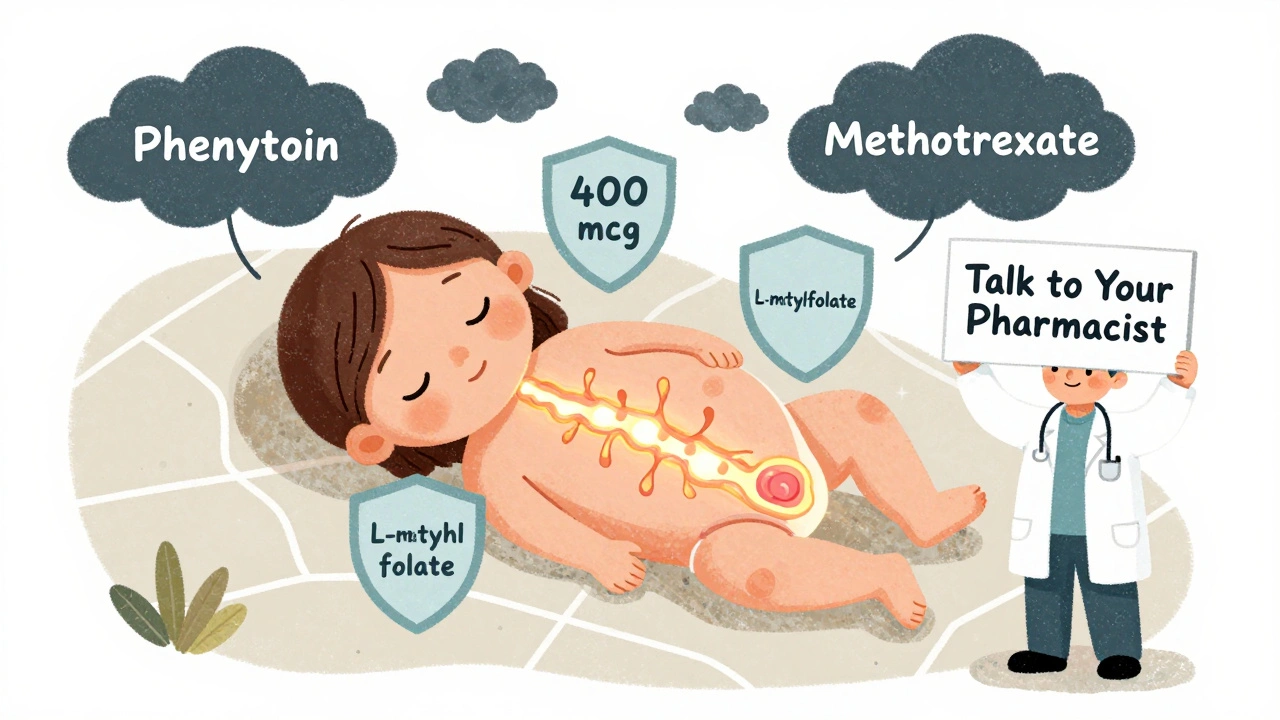
Folic acid is the synthetic form of folate, a B vitamin your body uses to make DNA and build new cells. During pregnancy, your baby’s nervous system is forming at lightning speed. Without enough folic acid, the risk of neural tube defects-like spina bifida or anencephaly-goes up dramatically. Studies show that taking 400 mcg daily before and during early pregnancy cuts that risk by 50 to 70%. The CDC has been pushing this message since 1992, and since the U.S. started fortifying flour with folic acid in 1998, NTD rates dropped by nearly half.
But here’s the catch: your body doesn’t absorb folic acid the same way it absorbs folate from food. Natural folate in spinach, lentils, or avocado has only about 50% bioavailability. Synthetic folic acid in supplements? Up to 100% if taken on an empty stomach. That’s why prenatal vitamins rely on folic acid, not food-based folate. Most contain 600 to 1,000 mcg-enough to meet the 600 mcg DFE daily recommendation for pregnant women.
Common Medications That Interfere with Folic Acid
It’s easy to assume that because folic acid is a vitamin, it’s harmless. But it’s not. Certain drugs react with it in ways that can be dangerous if you don’t know what you’re doing.
Anticonvulsants like phenytoin (Dilantin), carbamazepine (Tegretol), and valproic acid are the biggest red flags. These drugs lower folic acid levels in your blood. At the same time, high doses of folic acid can reduce the effectiveness of these seizure medications. One Reddit user, u/AnxiousMom2022, shared how she had a breakthrough seizure after starting a prenatal vitamin while on phenytoin. Her neurologist later confirmed: folic acid can antagonize anticonvulsant action. Women with epilepsy often need 4,000 to 5,000 mcg daily under strict supervision-far above the standard dose.
Methotrexate, used to treat ectopic pregnancies or autoimmune conditions, is another major interaction. It works by blocking folate metabolism. If you’re taking it, your doctor might prescribe folic acid to reduce side effects like nausea or liver damage-but timing is everything. Too much too soon can interfere with the drug’s intended effect. In some cases, doctors give folic acid 24 hours after methotrexate to avoid this.
Pyrimethamine, used for toxoplasmosis during pregnancy, also competes with folate. Adding folic acid can make it less effective. Pharmacists at CVS report that 32% of patients on this drug need dose adjustments when they start prenatal vitamins.
Sulfasalazine, often used for Crohn’s disease or ulcerative colitis, blocks folic acid absorption in the gut. The UK’s NICE guidelines warn that women on this drug must be monitored closely for folate deficiency during pregnancy. Left unchecked, it can lead to megaloblastic anemia and developmental issues.
What About Iron and Calcium in Prenatal Vitamins?
Most prenatal vitamins include iron and calcium because pregnant women need more of both. But here’s the problem: iron can reduce folic acid absorption by 20 to 30% when taken at the same time. Calcium does something similar-it can knock absorption down by 25% if you take them together with a glass of milk or a calcium supplement.
That’s why so many women on Reddit say they switched from a combined prenatal to separate supplements. One user wrote: “I was puking every time I took my prenatal. Switched to a folic acid-only pill in the morning and iron at night. No more nausea, and my OB said my folate levels are perfect.”
The fix? Take your prenatal vitamin with food to reduce stomach upset, but don’t pair it with calcium-rich meals or antacids. If you’re taking extra calcium or iron supplements, space them out by at least 2 to 3 hours. Some women find it easier to take folic acid on an empty stomach with water first thing in the morning, and iron after dinner.
Who Needs More Than 800 mcg?
The standard dose is 400 to 800 mcg. But some women need more.
- If you’ve had a previous pregnancy affected by a neural tube defect, your doctor will likely recommend 4,000 mcg daily, starting at least a month before trying to conceive.
- If you have diabetes, obesity, or are on anticonvulsants, higher doses may be needed.
- If you have the MTHFR C677T gene variant (found in 10-25% of people, especially Hispanics), your body converts folic acid to its active form poorly. In these cases, L-methylfolate (like Quatrefolic®) is a better choice. The FDA approved the first prenatal with this form in 2023, priced around $46/month.
Don’t up your dose on your own. Too much folic acid can hide a vitamin B12 deficiency, which can cause nerve damage. That’s why doctors check your B12 levels before prescribing high-dose supplements.
What You Shouldn’t Do
There are a few things that sound harmless but can mess with folic acid absorption:
- Don’t take it with antacids. They raise stomach pH, and folic acid needs acid to be absorbed. A Tums or Pepto right before your vitamin? That can cut absorption by half.
- Don’t rely on fortified foods alone. One slice of bread gives you 32 mcg. You’d need to eat 12 slices to hit 400 mcg. That’s not realistic-and you’d get too much sodium and sugar.
- Don’t assume all prenatal vitamins are the same. Some have only 400 mcg; others go up to 1,000 mcg. Check the label. If you’re on medication, your doctor might need to prescribe a specific brand.
What’s New in 2025?
The FDA is pushing to fortify corn masa flour with folic acid by 2025. Why? Hispanic women in the U.S. have 20-30% higher rates of neural tube defects. Corn tortillas and tamales are staples in many households, but they’re not currently fortified. This change could prevent hundreds of birth defects annually.
Research is also looking at whether folic acid lowers autism risk. A 2022 JAMA Pediatrics study of 45,300 children showed a 40% drop in ASD risk with periconceptional folic acid. But a 2021 Danish study found no link. The science isn’t settled yet-but the benefits for neural development are clear.
Bottom Line: What to Do Right Now
If you’re trying to get pregnant or already are:
- Start taking 400-800 mcg of folic acid daily, even if you’re not sure you’re pregnant.
- Check your prenatal vitamin label. Make sure it has at least 600 mcg.
- If you’re on any medication-especially for seizures, autoimmune disease, or cancer-tell your OB and pharmacist. Don’t assume it’s safe.
- If you have nausea from iron, take folic acid in the morning on an empty stomach and iron at night.
- Don’t take calcium or antacids within 2 hours of your folic acid.
- If you’ve had a previous NTD pregnancy or have MTHFR, ask about L-methylfolate.
Folic acid isn’t magic. But when used right, it’s one of the most powerful tools we have to prevent serious birth defects. The key isn’t just taking it-it’s taking it correctly, safely, and with full awareness of what else you’re putting in your body.
Can I get enough folic acid from food alone during pregnancy?
No. While foods like spinach, black beans, and fortified cereals contain folate, your body absorbs only about half of it. To reach the 600 mcg DFE needed during pregnancy, you’d need to eat over 2 cups of cooked lentils every day-plus a lot of other folate-rich foods. Supplements are the only reliable way to hit the target, especially since neural tube closure happens before most women know they’re pregnant.
Is it safe to take more than 1,000 mcg of folic acid daily?
Only under medical supervision. The upper limit is 1,000 mcg for adults over 18. Higher doses are used for women with epilepsy, previous NTD pregnancies, or MTHFR mutations-but they require close monitoring. Too much folic acid can mask a vitamin B12 deficiency, which can lead to permanent nerve damage. It may also lead to unmetabolized folic acid in the blood, though no direct harm has been proven yet.
Do prenatal vitamins with DHA affect folic acid absorption?
No. DHA (an omega-3 fatty acid) doesn’t interfere with folic acid. In fact, many prenatal vitamins combine both because they support brain development. The real culprits are iron, calcium, and antacids. If your prenatal has DHA and you’re tolerating it, there’s no need to switch unless you’re on other medications that interact with folate.
What’s the difference between folic acid and L-methylfolate?
Folic acid is synthetic and must be converted by your body into its active form, 5-MTHF. L-methylfolate (like Quatrefolic®) is already active, so your body doesn’t need to convert it. This matters if you have the MTHFR gene variant, which affects 1 in 5 people. If you’ve had trouble with standard folic acid or have a history of miscarriages or NTDs, L-methylfolate may be more effective.
Can I stop taking folic acid after the first trimester?
You can, but most doctors recommend continuing. While the neural tube closes by week 6, folic acid continues to support rapid cell growth, placental development, and red blood cell production throughout pregnancy. Stopping early increases your risk of anemia and may impact fetal growth. It’s safer to keep taking it unless your provider says otherwise.


Mindy Bilotta
December 3, 2025 AT 02:05just took my prenatal with a glass of milk and now i’m panicking 😅 guess i’m switching to morning folic acid + night iron. why is everything so complicated when you’re trying to grow a human??
Ethan McIvor
December 4, 2025 AT 22:54it’s wild how something so simple-like taking a pill-can have this whole ripple effect on your body, your meds, your peace of mind. i used to think vitamins were just… harmless candy. turns out they’re more like tiny surgeons with a checklist. 🤯
Palanivelu Sivanathan
December 6, 2025 AT 17:55THE SYSTEM IS DESIGNED TO KEEP YOU AFRAID!!
They don’t want you to know that folic acid is just a corporate scam to sell more pills!!
What if… the real solution is… sunlight??
AND WHY ISN’T ANYONE TALKING ABOUT THE TUMS FACTOR??
THEY’RE HIDING THE TRUTH IN THE LABELS!!
MY COUSIN’S NEPHEW’S DOG GOT A NEURAL TUBE DEFECT BECAUSE OF THIS!!
WE NEED A REVOLUTION!!
Adrianna Alfano
December 8, 2025 AT 02:02okay but why does every single prenatal vitamin in the US have iron in it??
my doctor said i should take them separately because i’m iron overload and i got yelled at by a pharmacist for asking if i could get a ‘folic acid only’ version like it was a crime.
also why is L-methylfolate $46 a month??
it’s a vitamin, not a luxury perfume.
someone’s making bank off our anxiety.
Casey Lyn Keller
December 9, 2025 AT 04:27so let me get this straight-folic acid helps prevent birth defects, but only if you don’t take it with calcium, iron, antacids, or your seizure meds… and you have to time it perfectly, and check your gene variant, and your OB doesn’t even know half this stuff…
and you’re supposed to trust this system?
yeah no thanks. i’m just eating spinach and hoping for the best.
Jessica Ainscough
December 10, 2025 AT 06:19i switched to L-methylfolate after my first miscarriage and honestly? it felt like my body finally stopped fighting me. no nausea, no brain fog. i didn’t know about MTHFR until my genetic test-now i wish i’d known years ago. if you’ve had losses or weird symptoms, ask for the test. it’s not expensive.
Katey Korzenietz
December 10, 2025 AT 17:45you people are overcomplicating this. just take the damn pill. if you’re on anticonvulsants, your doctor already knows. if you’re not, stop reading Reddit and go to a real doctor. this isn’t a TikTok trend. it’s medicine.
Brian Perry
December 10, 2025 AT 21:44wait wait wait-so if you take Tums with your prenatal… you’re basically sabotaging your baby’s brain development??
so every time i took a Tums for heartburn… was i… killing my future child??
oh god oh god oh god i took 12 Tums last week…
is it too late??
do i need to start praying to the Folic Acid Gods??
someone please tell me i didn’t do irreversible damage
Chris Jahmil Ignacio
December 12, 2025 AT 09:48they’ve been lying to us since 1998. the flour fortification? a cover. they don’t care about neural tube defects-they care about controlling your reproductive choices. folic acid is just the gateway drug to mandatory prenatal regimens. once you’re on it, you’re hooked. they’ll tell you to take more. then they’ll tell you to test your genes. then they’ll tell you to pay for expensive versions. then they’ll tell you to stop having kids if you’re ‘high risk.’ it’s a pipeline. and you’re the product.
Paul Corcoran
December 13, 2025 AT 08:44if you’re reading this and feeling overwhelmed-you’re not alone. this stuff is confusing even for doctors. the fact that you’re asking questions means you’re already doing better than most. take one step: check your vitamin label. call your pharmacist. ask if L-methylfolate is an option. you don’t need to fix everything today. just start somewhere. you’ve got this.
Colin Mitchell
December 14, 2025 AT 23:29my wife took 4000 mcg because of her epilepsy and it saved our daughter’s life. she had a seizure right before we knew she was pregnant. if we hadn’t been on high-dose folic acid, she might’ve lost the baby. don’t be afraid to ask for what you need. your doctor isn’t the only expert-your body knows too. trust yourself, and don’t let anyone make you feel silly for asking.