Most people don’t realize their kidneys are failing until it’s too late. That’s because chronic kidney disease (CKD) doesn’t scream for attention. No sharp pain. No fever. No obvious warning signs-until the damage is severe. By the time symptoms like fatigue, swelling, or nausea show up, the kidneys have already lost 70% or more of their function. And here’s the hard truth: 90% of people with CKD don’t know they have it. But it doesn’t have to be this way.
What Chronic Kidney Disease Really Means
| Stage | eGFR (mL/min/1.73m²) | Albuminuria Level | What It Means |
|---|---|---|---|
| G1 | 90 or higher | A2 or A3 | Normal function, but kidney damage is present |
| G2 | 60-89 | A2 or A3 | Mildly reduced function, damage confirmed |
| G3a | 45-59 | A2 or A3 | Mild to moderate loss; high risk of progression |
| G3b | 30-44 | A2 or A3 | Moderate to severe loss; 2.6x higher risk of failure |
| G4 | 15-29 | A2 or A3 | Severe loss; specialist care needed |
| G5 | Below 15 | A2 or A3 | Kidney failure; dialysis or transplant required |
Chronic kidney disease isn’t just about low kidney function. It’s about lasting damage. The official definition from KDIGO-used by doctors worldwide-says CKD is when your kidneys show signs of injury for at least three months. That could mean protein in your urine, abnormal imaging, or structural changes seen on a scan. Even if your eGFR looks normal, if you have persistent proteinuria, you still have CKD. And that’s where most people get confused.
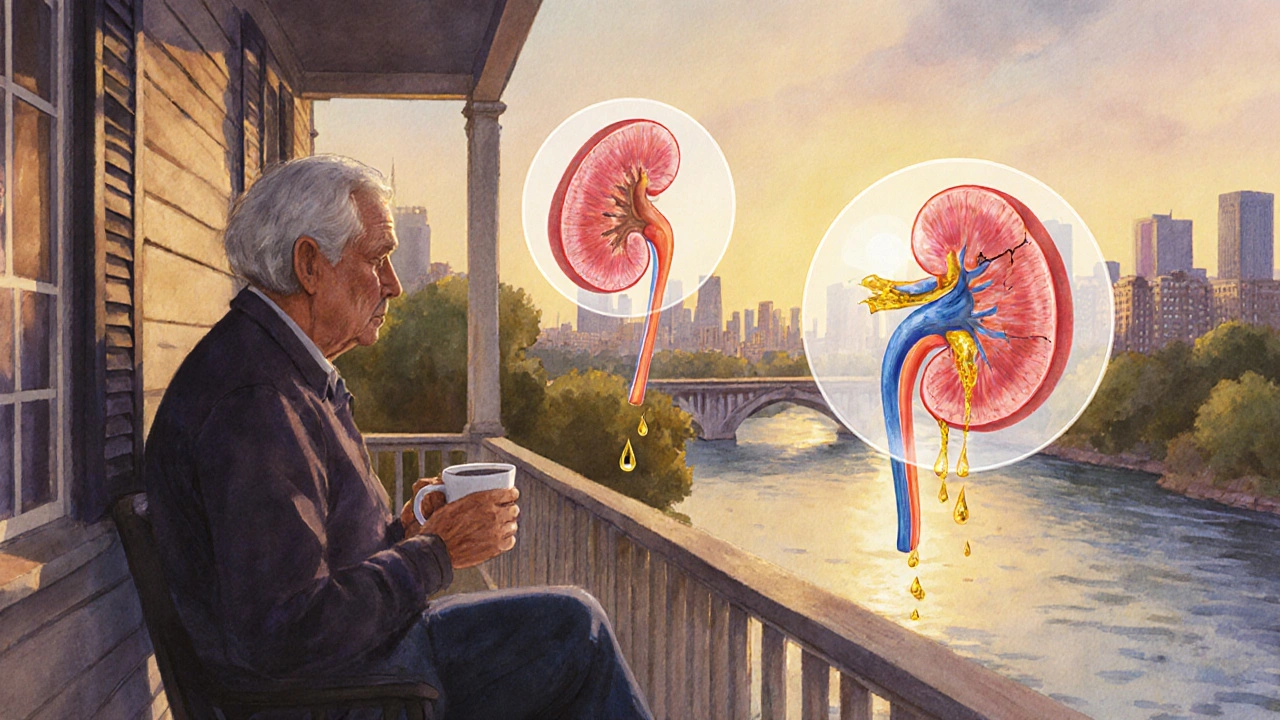
Think of it like high blood pressure. You don’t feel it until your heart is struggling. Same with kidneys. They’re quiet workers. They filter 120-150 quarts of blood every day. They balance your fluids, make red blood cell signals, and control your blood pressure. When they start failing, your body doesn’t scream-it just slows down. Fatigue? You blame it on stress. Swollen ankles? You think it’s from standing too long. That’s why so many are diagnosed by accident-during a routine check-up for a sprained ankle, a flu shot, or a diabetes screen.
How CKD Progresses-And Why It’s Not Always Linear
Not everyone with Stage G2 or G3a will end up on dialysis. That’s the myth. Progression isn’t guaranteed. It’s influenced by what you do next. Someone with Stage G3a and high albuminuria (A3) has a 2.6 times higher chance of hitting kidney failure within five years than someone with the same eGFR but low albuminuria (A1). That’s not just a number-it’s a call to action.
Diabetes and high blood pressure are the big two. Together, they cause over 60% of all CKD cases in the U.S. But here’s something less known: repeated kidney infections, certain medications like long-term NSAIDs (ibuprofen, naproxen), and even untreated sleep apnea can speed things up. And genetics? They matter too. African Americans are 3.5 times more likely to develop CKD than White Americans. Native Americans have the highest rates of diabetes-related kidney failure in the world.
One of the biggest mistakes? Assuming that a drop in eGFR always means disease. In older adults-especially over 70-a slower eGFR often reflects natural aging, not progressive kidney damage. That’s why doctors now look at trends over time. If your eGFR drops more than 5 mL/min/year, that’s a red flag. If it’s stable for two years? That’s not the same as active disease. This is why the KDIGO group debated whether Stage G3a should even be labeled as CKD for people over 70 with stable numbers and no protein in urine. Overdiagnosis can cause more harm than good-unnecessary anxiety, extra tests, even fear of normal aging.
Early Detection: It’s Not About Fear-It’s About Time
The real game-changer in CKD isn’t a new drug. It’s catching it early. Studies show that people diagnosed at Stage G3 or earlier have 32% better adherence to treatment and 41% more confidence managing their health. Why? Because they had time. Time to adjust their diet. Time to start blood pressure meds like ACE inhibitors or ARBs. Time to control blood sugar. Time to stop smoking. Time to learn what to avoid.
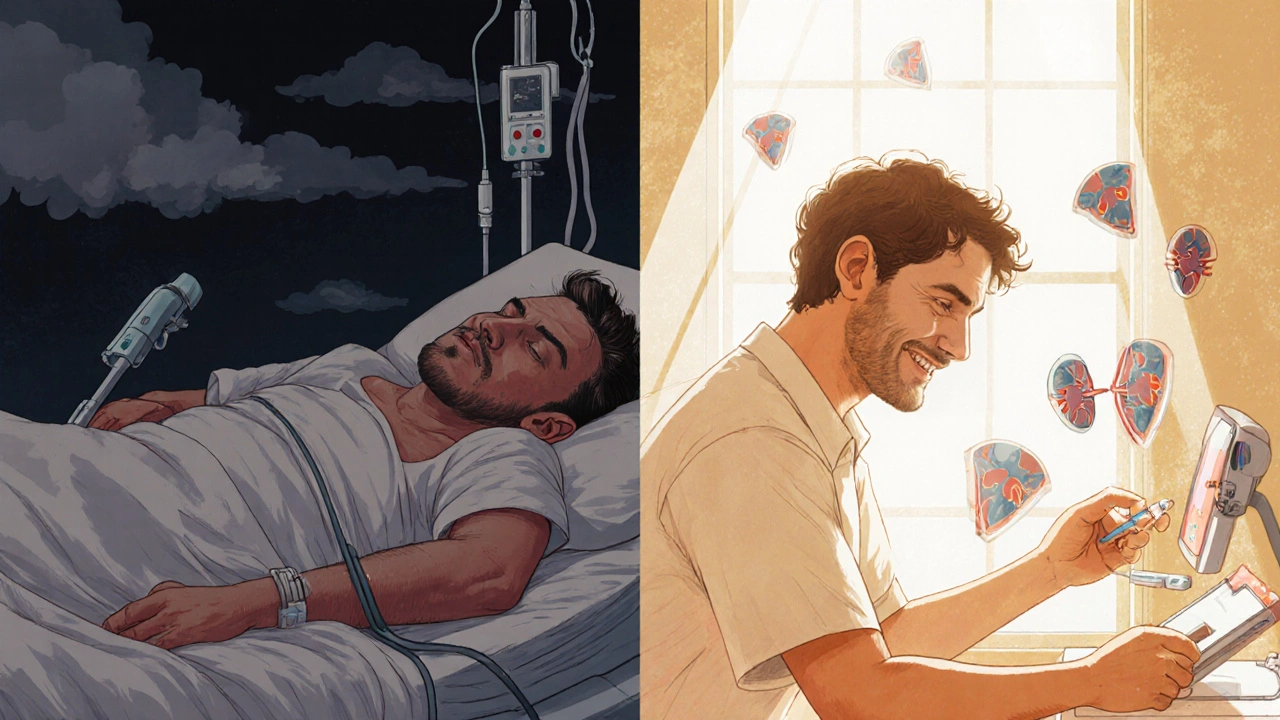
One patient, a nurse named Lisa from Ohio, was diagnosed at Stage G2 after a routine urine test for knee surgery. She had no symptoms-just occasional swelling she’d ignored. Her doctor put her on an ACE inhibitor and referred her to a dietitian. Five years later, her eGFR is still at 62. She’s not on dialysis. She’s not in crisis. She’s managing.
Compare that to a man from Texas who waited until he was exhausted, puffy, and vomiting. His eGFR was at 19. He needed emergency dialysis. He had no warning. No preparation. No chance to avoid it.
Here’s what early detection looks like in practice:
- Get a simple blood test for creatinine-this calculates your eGFR.
- Get a urine test for albumin-to-creatinine ratio (ACR). This catches protein leakage before it’s obvious.
- If either is abnormal, repeat the test in 90 days. One abnormal result isn’t enough.
- If both are abnormal over time? You have CKD. Now you know.
Doctors are getting better at this. Some clinics now use electronic alerts-when your eGFR drops below 60 and your ACR is over 30, the system flags it automatically. One study showed this boosted accurate diagnoses from 42% to 79% in just 18 months. But it’s not perfect. Many primary care providers still miss it. That’s why you need to be your own advocate.
Who Should Be Tested-and When
You don’t need to wait until you’re sick. If you have any of these, get tested every year:
- Diabetes (Type 1 or Type 2)
- High blood pressure (especially if you’re on medication)
- Heart disease
- Obesity (BMI over 30)
- A family history of kidney failure
- Are African American, Native American, or Hispanic
- Are over 60
Even if you don’t have any of those, if you’re taking NSAIDs daily (like for arthritis or back pain), or you’ve had repeated kidney infections, ask for a urine test. It’s quick. It’s cheap. It’s non-invasive.
And don’t ignore the new tools. The FDA just approved the first AI-based system-AION nephroTM-that predicts your risk of kidney decline over the next two years using 27 different data points: lab results, medications, age, BMI, even lab trends over time. It’s 88.7% accurate. It’s not in every doctor’s office yet-but it’s coming.
What Happens If You’re Diagnosed
Being told you have CKD doesn’t mean your life is over. It means you’ve been given a heads-up. And that’s rare in medicine.
At Stage G1 or G2, the focus is simple: protect what you’ve got. Control your blood pressure (target under 130/80). Keep blood sugar steady if you’re diabetic. Avoid NSAIDs. Cut back on salt. Eat more vegetables, less processed food. Drink water-but don’t overdo it. No special “kidney diet” yet-just smart eating.
At Stage G3a or G3b, things get more serious. Your doctor will likely start you on an ACE inhibitor or ARB. These aren’t just blood pressure meds-they directly protect your kidneys. Studies show they cut progression to Stage G4 by 37% in high-risk patients. You’ll also see a nephrologist. Not because you’re doomed-but because you need a specialist to help you plan ahead.
At Stage G4, you’re preparing for what’s next. Dialysis options. Transplant evaluation. Nutrition counseling. Mental health support. This is where many patients feel overwhelmed. But those who start early say the same thing: “I’m glad I had time to get ready.”
And at Stage G5? You need dialysis or a transplant to live. But even here, early detection changes outcomes. People who know they’re heading here have better outcomes than those who crash into it.
The Bigger Picture: Why This Matters Beyond You
CKD isn’t just a personal health issue. It’s a financial time bomb. Medicare spends $48 billion a year on dialysis and transplants. By 2030, that could hit $72 billion-if we don’t change course. Most of that cost comes from treating late-stage disease. Early detection and intervention could cut that bill by billions.
And it’s working. In Baltimore, a mobile screening program found over 1,200 people with early-stage CKD who didn’t know they had it. Most were in their 50s and 60s. Most had diabetes or high blood pressure. None had symptoms. Now they’re being monitored. They’re getting help. They’re not ending up on dialysis.
The future? Genomic testing. Within five years, your risk of kidney failure might be predicted by a simple DNA test that looks at 17 gene variants. That’s not sci-fi-it’s already in research labs. We’re moving from treating disease to predicting it.
But right now? The most powerful tool is still the simple blood test and urine test. No machine. No surgery. No cost. Just two samples. And a willingness to ask: “Could this be my kidneys?”
Can chronic kidney disease be reversed?
In early stages-G1 and G2-yes, progression can often be slowed or even stopped. Controlling blood pressure, managing diabetes, avoiding kidney-toxic drugs, and eating well can stabilize kidney function. But once significant scarring occurs (usually by Stage G3b), the damage is permanent. The goal shifts from reversal to slowing further decline.
What’s the difference between eGFR and creatinine?
Creatinine is a waste product your muscles make. Your kidneys filter it out. A blood test measures how much creatinine is in your blood. But that number alone doesn’t tell you how well your kidneys are working. eGFR (estimated glomerular filtration rate) is a formula that uses your creatinine level, age, sex, and race to estimate how much blood your kidneys filter each minute. It’s the best single number doctors use to track kidney function.
Why does albumin in urine matter so much?
Healthy kidneys don’t let protein like albumin leak into urine. When albumin shows up, it means the filters are damaged. Even if your eGFR is normal, albuminuria is a sign of early kidney injury. People with high albumin levels (A3) have more than five times the risk of dying from kidney or heart disease compared to those with normal levels, regardless of their eGFR.
Can I still drink alcohol if I have CKD?
Moderate alcohol-like one drink a day for women, two for men-is usually okay if your kidneys are stable and you don’t have liver disease. But heavy drinking raises blood pressure and can damage kidneys faster. If you’re in Stage G3 or higher, your doctor may recommend cutting back or stopping entirely.
Do I need to stop taking ibuprofen or naproxen?
Yes, if you have CKD, especially Stage G3 or higher. These NSAIDs reduce blood flow to the kidneys and can cause sudden, dangerous drops in kidney function. Tylenol (acetaminophen) is usually safer for pain relief-but always check with your doctor first.
Is there a cure for chronic kidney disease?
There’s no cure once significant damage is done. But a kidney transplant can restore normal function and is the closest thing to a cure. For many, it means returning to a near-normal life. However, transplant isn’t for everyone. Prevention and early management remain the most effective strategies.
Can I still exercise with CKD?
Yes-exercise is one of the best things you can do. Regular physical activity helps control blood pressure, improves heart health, and reduces inflammation. Aim for 30 minutes of walking, swimming, or cycling most days. Talk to your doctor about what’s safe for your stage. Avoid heavy weightlifting if you’re on dialysis or have fluid overload.
What foods should I avoid with CKD?
In early stages, focus on reducing sodium, processed foods, and added sugars. As CKD advances, you may need to limit potassium (bananas, potatoes, oranges) and phosphorus (dark sodas, processed cheese, processed meats). But don’t start a restrictive diet without guidance. A kidney dietitian can help you tailor your meals to your stage and lab results.
If you’re over 50, have high blood pressure or diabetes, or just feel like something’s off-don’t wait for symptoms. Ask your doctor for an eGFR and ACR test. It takes five minutes. It could save your kidneys. And maybe, your life.

swatantra kumar
November 20, 2025 AT 03:45Dave Wooldridge
November 21, 2025 AT 20:21Sarah Swiatek
November 23, 2025 AT 16:24rob lafata
November 25, 2025 AT 12:36Matthew McCraney
November 26, 2025 AT 03:37Nick Naylor
November 27, 2025 AT 21:31Brianna Groleau
November 29, 2025 AT 10:58Rebecca Cosenza
November 30, 2025 AT 17:29Cinkoon Marketing
December 2, 2025 AT 08:19robert cardy solano
December 3, 2025 AT 04:08Rusty Thomas
December 3, 2025 AT 23:43