Pharmacy Benefit Manager: How It Controls Your Drug Costs and What You Need to Know
When you pick up a prescription, the price you see isn’t set by your doctor or pharmacy—it’s often decided by a pharmacy benefit manager, a middleman that negotiates drug prices between insurers, pharmacies, and drug makers. Also known as PBM, it’s the hidden force behind why some pills cost $5 and others $500, even if they’re the same drug. Most people don’t realize PBMs control nearly 80% of prescription drug spending in the U.S. They don’t make medicine, but they decide which drugs get covered, which pharmacies you can use, and how much you pay out of pocket.
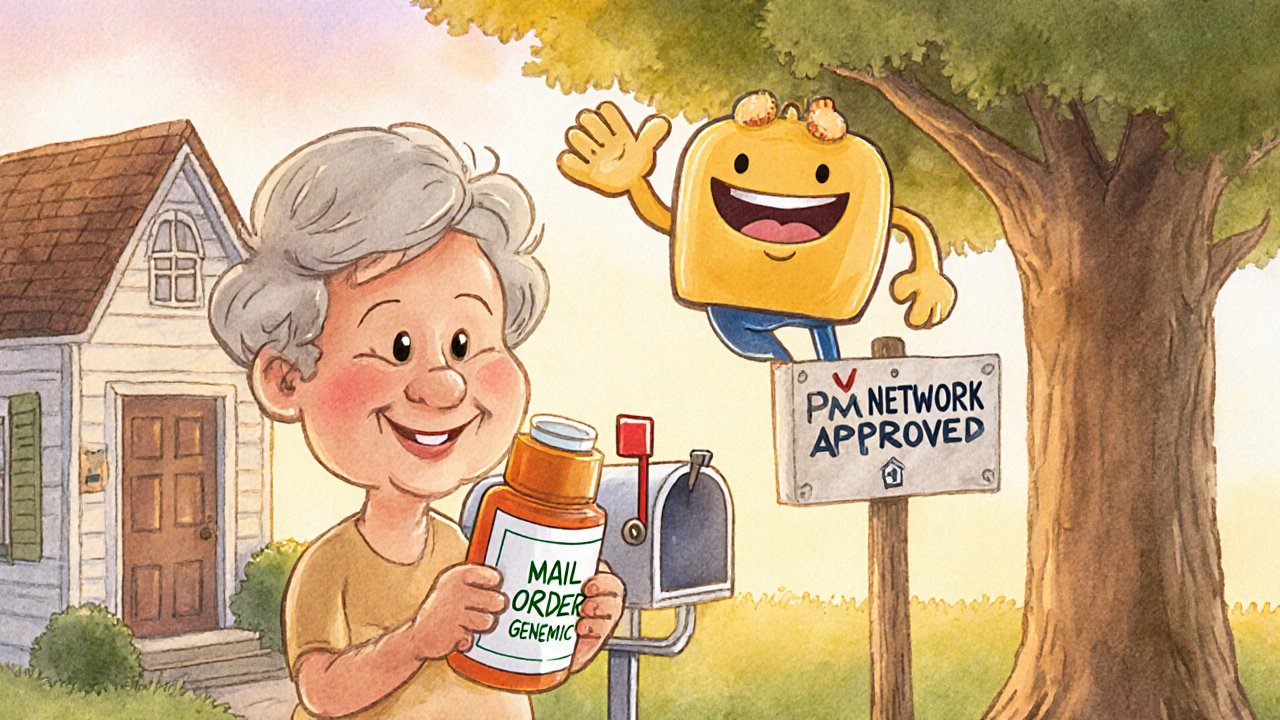
Here’s how it works: PBMs strike deals with drug companies. If a company pays them a big rebate, the PBM puts that drug on the preferred list—meaning your insurance covers it cheaply. But if the drug doesn’t pay up, it gets pushed to a higher tier, and you pay more. This is why generic versions sometimes cost more than brand names—because the brand pays the PBM a bigger cut. PBMs also own or partner with mail-order pharmacies, which means your local pharmacy might not even be allowed to fill your script unless the PBM approves it. And if you’ve ever been told your drug is "not covered" or you need prior authorization, that’s the PBM pulling the strings.
It’s not just about price—it’s about access. A pharmacy benefit manager, a middleman that negotiates drug prices between insurers, pharmacies, and drug makers can delay or block life-saving drugs by making them too expensive or requiring unnecessary paperwork. That’s why you’ll find articles here on generic drug quality, manufacturing flaws in overseas plants leading to recalls and shortages, and why some seniors are stuck with high-risk medications, drugs that increase fall risk and confusion in older adults—because PBMs pushed cheaper, riskier options to save money. You’ll also see how drug recalls, official alerts from the FDA about unsafe medications are handled—or ignored—by these companies.
What you’ll find below isn’t just theory. It’s real stories from people who got hit with surprise bills, had their meds switched without warning, or couldn’t get a refill because their PBM changed the rules overnight. From how medication refills abroad, getting prescriptions filled while traveling internationally get tangled in PBM networks, to why OTC cold medicine, common over-the-counter drugs like Sudafed can be dangerous if your PBM didn’t flag a drug interaction, this collection cuts through the jargon. You’ll learn how to spot when a PBM is working against you—and what you can do to fight back.
Insurance Coverage of Online Pharmacy Generics: What You Need to Know in 2025
Learn how insurance covers generic drugs from online pharmacies in 2025 - including mail-order vs. independent sites, copay differences, and how to avoid costly mistakes.
READ MORE