Insurance Coverage: What You Need to Know About Drug Costs and Access
When it comes to insurance coverage, the system that determines which medications your plan will pay for and how much you’ll pay out of pocket. Also known as pharmacy benefits, it’s not just about having health insurance—it’s about knowing what’s actually covered under your plan. Many people assume their insurance means free or cheap drugs, but that’s not always true. High copays, prior authorizations, step therapy, and formulary restrictions can turn a simple prescription into a bureaucratic headache. Even if your plan lists a drug as covered, it might only cover the generic version, or require you to try cheaper alternatives first. This is why understanding your insurance coverage isn’t optional—it’s essential for managing chronic conditions, avoiding treatment gaps, and preventing unexpected bills.
Prescription drug costs, the amount you pay for medications after insurance applies, can vary wildly even for the same drug. A 30-day supply of a common medication might cost $5 with one plan and $80 with another, depending on tier placement, pharmacy network, and whether it’s on a preferred list. Some plans don’t cover certain drugs at all, especially newer or specialty medications. For example, a drug like Avandia or Vidalista might be covered under one insurer but require a lengthy appeal under another. Medication access, your ability to get the right drug at the right time, is directly tied to how your insurer structures its formulary. If your doctor prescribes a medication that’s not on your plan’s list, you might be stuck paying full price, switching to a less effective alternative, or fighting through paperwork for an exception.
And it’s not just about the drug itself. Drug affordability, how easily you can sustain the cost of treatment over time affects whether you skip doses, split pills, or stop taking medication altogether. Studies show that people on high-deductible plans are more likely to delay filling prescriptions for conditions like diabetes or high blood pressure—leading to worse outcomes down the line. That’s why knowing your plan’s deductible, out-of-pocket maximum, and tiered co-pays matters as much as knowing what’s covered. If you’re managing a long-term condition like chronic kidney disease or metabolic syndrome, even small changes in coverage can have big consequences for your health and budget.
What you’ll find below are real, practical guides that cut through the noise. From how to verify if your medication is covered to what to do when your insurer denies a claim, these posts give you the tools to navigate the system. You’ll learn how insurance rules affect your access to common drugs like Bactrim or Claritin, why some medications require prior authorization, and how to spot when a generic drug might be unsafe due to manufacturing issues. Whether you’re a senior managing multiple prescriptions, a traveler needing refills abroad, or someone just trying to afford their daily meds, this collection gives you the clarity you need to take control.
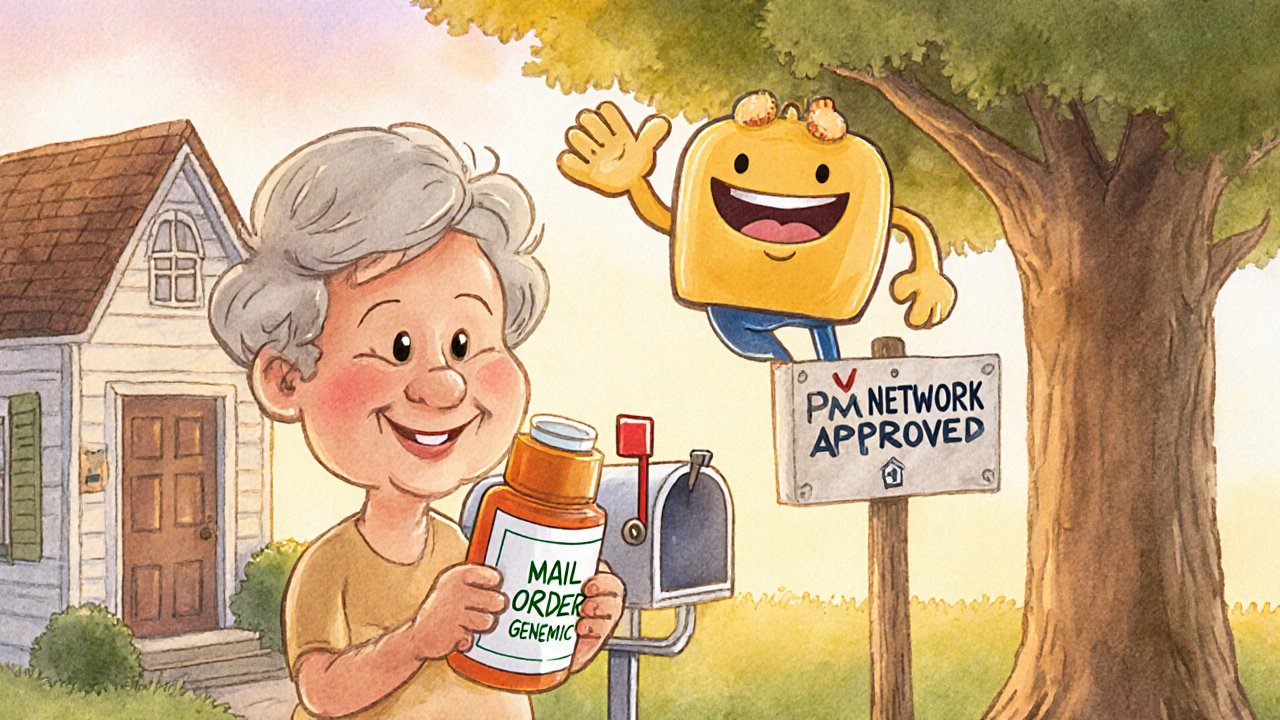
Insurance Coverage of Online Pharmacy Generics: What You Need to Know in 2025
Learn how insurance covers generic drugs from online pharmacies in 2025 - including mail-order vs. independent sites, copay differences, and how to avoid costly mistakes.
READ MORE